NEW in 2016, Special Symposia are not-to-be-missed presentations led by leading researchers and clinicians.
Identified by the ACRM Program Committee, SPECIAL SYMPOSIA refer to one or more symposium in each block of concurrent sessions, and luncheon lectures that have extra-wide appeal
FOCUS AREA ABBREVIATIONS: AN: Arts & Neuroscience, BI: Brain Injury, CAN: Cancer, CC: Cross-Cutting, CP: Clinical Practice, DI: Diagnosis Independent, GER: Geriatric Rehabilitation, INT: International, MES: Measurement, MIL: Military/VA, ND: Neurodegenerative Diseases, NP: Neuroplasticity, PAIN: Pain Rehabilitation, PED: Pediatric Rehabilitation, POL: Health Policy & Legislation, SCI: Spinal Cord Injury, ST: Stroke, TEC: Technology
BLOCK 1
WED 2 NOV // 11:00 AM – 12:15 PM
Concussion, Traumatic Brain Injury, and Chronic Traumatic Encephalopathy: New Insights From the Battlefield, Gridiron, and Lab Bench #533 BI, MIL
Featuring Faculty: Lee Goldstein
Moderator: Douglas Katz
Emerging research supports links between repetitive concussive and subconcussive head injuries (contact sports, accidents, blast exposure) and long-term cognitive and neuropsychiatric problems, and increased risk for neuropathological sequelae, including chronic traumatic encephalopathy (CTE). The first part of the presentation will highlight neuropathological evidence of CTE in the first case series of postmortem brains from blast-exposed veterans compared to brains of young athletes with confirmed CTE. The second part will highlight experimental results from new mouse models of blast and impact TBI. Blast-exposed mice also exhibit evidence of CTE-linked neuropathology. Kinematic analysis and biomechanical modeling have revealed similarities and differences between blast and impact neurotrauma that inform clinical understanding of concussion, TBI, and CTE.

Lee Goldstein
Lee E. Goldstein, MD, PhD
Associate Professor of Psychiatry, Neurology, Ophthalmology, Pathology & Laboratory Medicine, Biomedical Engineering, Electrical & Computer Engineering
Dr. Goldstein is Director of the Molecular Aging & Development Laboratory, Center for Biometals & Metallomics, and the Neurotrauma Laboratory at Boston University School of Medicine and College of Engineering. Dr. Goldstein received medical (MD) and doctoral degrees (PhD, Neuroscience) from Yale as an NIH MSTP Scholar. He moved to Harvard in 1994 where he completed a clinical fellowship in psychiatry at Massachusetts General Hospital and research fellowships in molecular neurobiology (with Rudolph Tanzi) and ocular biology (with Leo Chylack). He established his laboratory as an NIH-AFAR Beeson Scholar and Assistant Professor in Psychiatry at Harvard where he remained until his recruitment to Boston University in 2008.
Recently, he and his team uncovered mechanisms subserving blast-related neurotrauma (“shell shock”) and links to chronic traumatic encephalopathy (CTE; Science Transl Med, 2012). He and his team collaborated on a promising new treatment for traumatic brain injury (TBI) and its aftermath (Nature, 2015). His current research focuses on understanding the mechanisms that determine and distinguish concussion, TBI, and CTE. Dr. Goldstein is an inventor on numerous patents derived from his research. He has received awards for his research from the NIH, American Federation for Aging Research, Alzheimer’s Association, Optical Society of America, Harvard Medical School, and Oxford University.

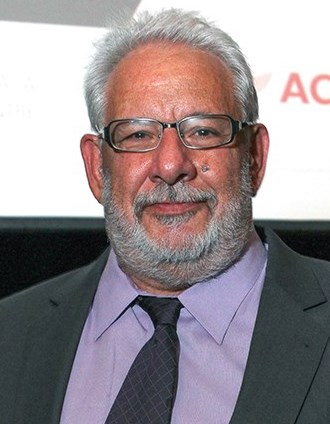
Douglas Katz
Douglas I. Katz, MD, FACRM, FAAN
Professor of Neurology, Boston University School of Medicine
Attending Neurologist, Boston Medical Center; Staff Neurologist, Boston
University Neurology Associates
Braintree Rehabilitation Hospital
Douglas I. Katz, MD is Professor of Neurology at Boston University School of Medicine, a member of the academic neurology staff at Boston Medical Center and Medical Director of the Brain Injury Program at Braintree Rehabilitation Hospital in Massachusetts. With subspecialties in cognitive/behavioral neurology and neurorehabilitation, he is a recognized expert and leader in the field of traumatic brain injury (TBI) rehabilitation with over 29 years of experience in TBI clinical care, clinical research, education and program development.
His research and publications have included studies of neuropathology, natural history and outcome prediction in TBI, disorders of consciousness after brain injury, pharmacologic treatment of cognitive problems after TBI, and structural and functional imaging in relation to recovery and rehabilitation after TBI. Dr. Katz has served on a number of boards of organizations involved in brain injury and neurorehabilitation including the American Congress of Rehabilitation Medicine, Brain Injury Association of America, American Society of Neurorehabilitation and MAB Community Services. He is President of the American Congress of Rehabilitation Medicine, 2015-2017.
SEE NONSTOP PROGRAM FOR BRAIN INJURY >>>
SEE NONSTOP PROGRAM FOR MILITARY / VA >>>
BLOCK 2

Mark D’Esposito
WED 2 NOV // 2:15 PM – 3:30 PM
The Modular Brain: Implications for Rehabilitation #867 NP, ST, BI
Featuring Mark D’Esposito MD, Professor of Neuroscience and Psychology and Director of the Henry H. Wheeler Jr. Brain Imaging Center at the University of California, Berkeley.
The brain is widely assumed to be a modular system. In this talk, I will discuss a series of empirical findings from functional MRI studies that begin to elucidate the neural architecture of modular processing by showing that brain modules execute discrete processes and connector hubs are likely integrating and sending information across modules in support of goal-directed cognition. I will also discuss how a better understanding of this type of large scale organization of the brain may lead to new approaches in the diagnosis, treatment and rehabilitation of neurological and psychiatric (or cognitive) disorders.
SEE NONSTOP PROGRAM FOR NEUROPLASTICITY >>
BLOCK 3
WED 2 NOV // 4:30 PM – 5:45 PM

Armin Curt
Recovery of Locomotor Function in SCI: How the Brain and Spinal Cord Interacts #1016 SCI
Featuring: Armin Curt, MD, FRCPC
Dr. Curt is the medical director of the Spinal Cord Injury Center at the University Hospital Balgrist and professor of paraplegiology at the University of Zuerich, Switzerland.
Recovery of walking function after neurotrauma, e.g. after spinal cord injury, is routinely captured using standardized walking outcome measures of time and distance. However, these measures do not provide information on possible underlying mechanisms of recovery, nor do they tell anything about the quality of gait. Patients with an incomplete spinal cord injury are a very heterogeneous group of patients with a wide range of functional impairments. A stratification of these patients would allow increasing sensitivity for hypothesis testing and a more targeted treatment strategy. Understanding the interaction between the brain and spinal cord in controlling locomotor function and how these interactions might be modified and facilitated during rehabilitation will be of importance to advance locomotor training. This will be also essential to inform clinical trials and targeting the stratification and rehabilitation protocols to most suitable patients and increase the effectiveness of interventions.
Learning objectives:
-To recognize impaired gait pattern in SCI
-What is impaired in lower limb motor control
-Contribution of the brain and cord to gait
-How recovery occurs in gait control and performance
PANELISTS
Prithvi Shah, PhD
Assistant Professor, Health and Rehabilitation Sciences, School of Health Technology and Management and Assistant Professor, Department of Neurobiology and Behavior, Stony Brook University
Edelle Field-Fote, PT, PhD, FAPTA
Director, Spinal Cord Injury Research & The Hulse Spinal Cord Injury Laboratory, Shepherd Center; Professor, Emory University School of Medicine, Division of Physical Therapy; Professor, Georgia Institute of Technology, School of Biological Sciences
T. George Hornby, PT, PhD
Professor, Department of Physical Medicine and Rehabilitation,
Indiana University School of Medicine; Research Scientist, Locomotor Recovery Laboratory, Sensory Motor Performance Program, Rehabilitation Institute of Chicago
SEE NONSTOP PROGRAM FOR SCI >>>
BLOCK 4
THU 3 NOV // 11:15 AM – 12:30 PM
The Public Health Approach to Traumatic Brain Injury #146 BI, POL
Featuring: Juliet K. Haarbauer-Krupa, Jeneita Bell, Mathew Breiding and Lara Depadilla

Juliet Haarbauer Krupa

Jeneita Bell

Mathew Breiding

Lara Depadilla
The public health model provides a framework for understanding a broader impact of TBI. This symposium will highlight key areas of focus at the Centers for Disease Control and Prevention to better describe the public health burden of TBI and to identify approaches to improve outcomes for those who experience TBI.
Juliet K. Haarbauer-Krupa, PhD, Health Scientist, Traumatic Brain Injury Team, Division of Unintentional Injury, National Center for Injury Prevention and Control, Centers for Disease Control; Adjunct, Faculty, Department of Pediatrics, Emory University School of Medicine
LCDR Jeneita Bell, MD, MPH
Medical Officer, Traumatic Brain Injury (TBI) Team, Division of Unintentional Injury Prevention National Center for Injury Prevention and Control, Centers for Disease Control and Prevention
Mathew Breiding, PhD
Behavioral scientist and team lead, Traumatic Brain Injury Team, Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention
Lara DePadilla, PhD is a Behavioral Scientist on the Traumatic Brain Injury Team in the National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention (CDC). She is currently the project lead for the TBI Surveillance System project.
SEE NONSTOP PROGRAM FOR BRAIN INJURY >>>
SEE NONSTOP PROGRAM FOR HEALTH POLICY >>>
BLOCK 5
THU 3 NOV // 4:45 PM – 6:00 PM

Exercise for the Elderly and People With Neurodegenerative Disease #860 ND, GER
Featuring Daniel Corcos, PhD, Northwestern University, Physical Therapy and Human Movement Sciences
It is now axiomatic that exercise is beneficial for everyone. For individuals experiencing physical and mental decline, as well as those suffering from neurodegenerative disease, exercise is considered medicine. This presentation will provide the general prescription for exercise, both for the elderly and those with neurodegenerative disease. The benefits of resistance training, endurance training and balance training will be outlined. The presentation will also discuss different approaches to working with the elderly. Finally the presentation will review recent studies on the benefits of exercise programs that target both the person being cared for and the caregiver.
Dr. Corcos is a motor systems neuroscientist working on “human electrophysiology” using TMS, fMRI, EEG, EMG as well as neuronal recordings in patients undergoing brain surgery. The primary goal of his research is to understand the mechanisms underlying therapeutic interventions for people with Parkinson’s disease.
SEE NONSTOP PROGRAM FOR NEURODEGENERATIVE DISEASES >>
SEE NONSTOP PROGRAM FOR GERIATRIC REHAB >>>
BLOCK 6
FRI 4 NOV // 10:00 AM – 11:15 AM
Let’s Think: Conceptualizations of Cognitive Rehabilitation #866 BI
Featuring Keith Cicerone, Deirdre Dawson and McKay Moore Sohlberg
This Special Symposium will address the concept of “contextualization” as it relates to cognitive rehabilitation. This concept is derived from the Institute of Medicine Report on Cognitive Rehabilitation Therapy for Traumatic Brain Injury that identified Contextualized and Decontextualized Treatments according to the degree to which they take place in the real world or use materials and tasks from the patient’s everyday life. This concept has implications for the design of interventions, selection of candidates, identification of effective ingredients (e.g., errorfull versus errorless learning), reliance on insight and self-awareness, and assumptions underlying the transfer and generalization of interventions. This concept also requires an understanding of the therapist’s active involvement and role in making explicit the relation of the intervention (especially the patient’s awareness of deficits and use of compensatory strategies) to the patient’s real-life functioning and active promotion of generalization (e.g. through multiple exemplars of strategy use). The conceptualization of cognitive rehabilitation will be explored in relation to assumptions underlying acontextualized, quasi-contextualized and fully contextualized forms of intervention.
Keith Cicerone
Keith Cicerone, PhD, ABPP-Cn, FACRM
Director of Neuropsychology & Rehabilitation Psychology and Clinical Director of the Cognitive Rehabilitation Department, JFK-Johnson Rehabilitation Institute and New Jersey Neuroscience Institute, JFK Medical Center
Project Director, New Jersey Traumatic Brain Injury Model System
Clinical Professor of Physical Medicine and Rehabilitation, University of Medicine and Dentistry of New Jersey
Associate Professor of Neuroscience, Seton Hall University Graduate School of Medical Education
Dr. Cicerone’s research has addressed the development and validation of interventions for impairments of attention and executive functioning after traumatic brain injury, and controlled trials of holistic neuropsychological rehabilitation. He is the primary author of three evidence-based reviews of cognitive rehabilitation after traumatic brain injury and stroke, conducted through the Brain Injury Interdisciplinary Special Interest Group of ACRM.

Deirdre Dawson
Deirdre R. Dawson, PhD, OT Reg. (Ont.)
Associate Professor, Department of Occupational Science & Occupational Therapy, & Rehabilitation Sciences Institute, University of Toronto
Senior Scientist, Rotman Research Institute, Baycrest Health Sciences, Toronto
Adjunct Scientist, Toronto Rehabilitation Institute, Toronto
Dr. Dawson is an Associate Professor in the Department of Occupational Science & Occupational Therapy at the University of Toronto. Her research focuses on developing and evaluating interventions for people with cognitive impairments that promote their autonomy and participation in every-day life.

McKay Sohlberg
McKay Moore Sohlberg, PhD, CCC-SLP
Communication Disorders & Sciences, University of Oregon
Dr. Moore Sohlberg is an Endowed Professor and Director of the Communication Disorders & Sciences Program at University of Oregon, and an ASHA Fellow. Dr. Sohlberg has published numerous articles, textbook, chapters, and manuals on managing cognitive impairments following acquired brain injury, and is a renowned researcher in the field.
BLOCK 7
FRI 4 NOV // 1:15 PM – 2:30 PM
SPECIAL SYMPOSIA: Music, Movement + the Mind in Rehabilitation #998
Featuring Ron Hirschberg, Brian Harris , Pamela Quinn and Ben Folds
In celebration of the newly formed Arts & Neuroscience Community group within ACRM and to showcase emerging studies and data on music & rhythm on healing, ACRM is proud to announce this fascinating session.
- Not your ordinary educational session…
- Multidisciplinary demonstration & lecture
- Showcasing emerging studies and data on music & rhythm on healing
- Neuroscience is explaining why music can aide in recovery, and how music can be used in rehabilitation

Ron Hirschberg, MD
Assistant Professor, Department of Physical Medicine & Rehabilitation
Spaulding Rehabilitation Hospital, Harvard Medical School

Brian Harris, MA, MT-BC, NMT/F
Neurologic Music Therapist
MedRhythms, Inc., Spaulding Rehabilitation Hospital
 Ben Folds is widely regarded as one of the major music influencers of our generation.
Ben Folds is widely regarded as one of the major music influencers of our generation.
He’s spent over a decade sharing the stage with some of the world’s greatest symphony orchestras – from Sydney, Australia to the Kennedy Center, performing his pop hits and his critically acclaimed concerto for Piano and Orchestra.
For five seasons he was a judge on the popular NBC series “The Sing Off,” which catapulted the art of a cappella into the national spotlight, and helped launch the careers of numerous a cappella groups.
Throughout his career, Folds has created an enormous body of genre-bending musical art that includes pop albums as the front man for Ben Folds Five, multiple solo rock albums, as well as unique collaborative records with artists from Sara Bareilles and Regina Spektor, to Weird Al and William Shatner. His most recent album is a blend of pop and classical original works, in part recorded with the revered classical sextet yMusic that soared to #1 on both the Billboard classical and classical crossover charts.
Beginning this fall, Folds will be back to pound pianos again with cross country solo touring reminiscent of his earliest solo tours, where he defied skeptics by delivering a high energy rock performance using the intimacy of just a piano.
 Pamela Quinn is a professional dancer who has had Parkinson’s disease (PD) for twenty years. Her personal experience of PD combined with her keen knowledge of the body derived from dance training gives her a unique position from which to analyze patients’ physical functioning and to imagine creative solutions to the problems posed by PD. Using a combination of cuing systems, music, dance, athletic drills, imagery and physical strategies, she gives people concrete tools to improve mobility. She also trains people to use their environments to help them with their symptoms. Her innovative approach has gained growing recognition and made her a sought out movement therapist, teacher and speaker in the PD community. She thinks of herself as a PD coach.
Pamela Quinn is a professional dancer who has had Parkinson’s disease (PD) for twenty years. Her personal experience of PD combined with her keen knowledge of the body derived from dance training gives her a unique position from which to analyze patients’ physical functioning and to imagine creative solutions to the problems posed by PD. Using a combination of cuing systems, music, dance, athletic drills, imagery and physical strategies, she gives people concrete tools to improve mobility. She also trains people to use their environments to help them with their symptoms. Her innovative approach has gained growing recognition and made her a sought out movement therapist, teacher and speaker in the PD community. She thinks of herself as a PD coach.
Quinn was the subject of a profile on the CBS Evening News with Katie Couric and featured in a piece by WABC in New York. Her writing has been published by Neurology Now, On the Move and Dance Magazine, for which she wrote a feature article on her experience as a dancer who developed a life-altering movement disorder. In addition to her private practice as a movement consultant, she regularly teaches both for PD Movement Lab, a class she originated and which is sponsored by the Brooklyn Parkinson Group, and for NYU’s Edmund J. Safra’s Wellness Program for PD at the JCC in NYC.
Professional engagements include venues such as NYU, U Penn, University of Maryland, Rutgers University, Atlanta’s Southeastern PD Conference, St. Louis and keynote presentations for Houston’s HAPS program, the New England Biennial PD Conference, and Connecticut’s MADPA program at the University of Hartford. She has collaborated with David Leventhal on lecture/demonstrations for the New York Academy of Medicine, Brown University, Columbia’s Narrative Medicine Program and the Center for Narrative Practice.
For both the second and third World Parkinson Congresses, she has been a teacher, panelist, and moderator and her video, “Welcome to our World” won their video competition in addition to receiving a Dance Media award. Her second video, “With Grace” was featured at the third World Parkinson Congress, and her most recent video, “Neurodance” (a rhythmized version of a neurology exam) has been received with acclaim.
Recent live performances include two works for people with PD: Three Sheets to the Wind, and The Matisse Project for MOMA. In film, she was a consultant to Christopher Walken who played a cellist with Parkinson’s in “A Late Quartet” and she appeared in the movie briefly herself. Pamela is a graduate of PDF’s Clinical Research Learning Institute, the Applied Teacher Training Program, author of Coping Strategies to Manage your Parkinson’s and creator of the DVD “Smart Moves with Pamela Quinn.” She lives in Manhattan with her husband and two children.









