Pre- & Post-Conference Courses
CME/CEU credit is included in the cost of every pre- and post-conference course listed here, except as noted. Credits are available in your choice of 11 disciplines. Maximize your educational experience and dig deep into areas of special interest by adding pre- and post-conference courses to your core conference registration. Whether you wish to squeeze in a few extra hours or pile on the CME/CEU credits, ACRM offers a tremendous selection of topics from which to choose.
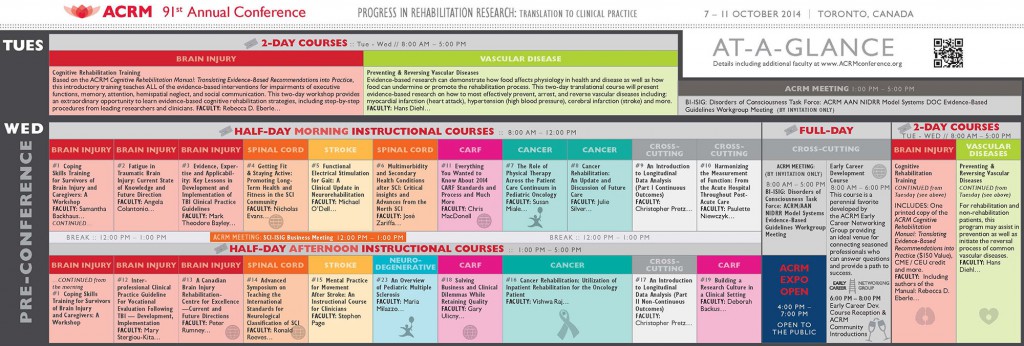
At-a-glance Pre-Conference Courses:
[sm_hr]
TWO-DAY COURSES // TUE AND WED // 7 – 8 OCTOBER
COGNITIVE REHABILITATION TRAINING
Tue & Wed // 7 – 8 OCTOBER
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
|
|
|
|
Faculty
Rebecca D. Eberle, MA, CCC-SLP, BC-NCD
Indiana University, Indianapolis, IN
Kristine T. Kingsley, PhD
Rusk Institute of Rehabilitation Medicine, New York, NY
Amy Shapiro-Rosenbaum, PhD
Park Terrace Care Center, Flushing, NY
Based on the ACRM Cognitive Rehabilitation Manual: Translating Evidence-Based Recommendations into Practice, this introductory training teaches ALL of the evidence-based interventions for impairments of executive functions, memory, attention, hemispatial neglect, and social communication. Learn more about the Manual.
Led by authors of the Manual, this two-day workshop provides an extraordinary opportunity to learn evidence-based cognitive rehabilitation strategies, including step-by-step procedures from leading researchers and clinicians in the field. View CME/CEU details and accreditation statements.
Registration Includes:
- Two days of live training with authors of the manual
- One printed copy of the ACRM Cognitive Rehabilitation Manual: Translating Evidence-Based Recommendations into Practice ($150 Value)
- CME / CEU Credit
- 6 months of online access to a previously recorded Cognitive Rehabilitation Training ($395 value)
- Non-member registration includes a 6-months Introductory Membership to ACRM
Who Should Attend?
- Occupational therapists
- Speech-language therapists
- Neuropsychologists
- Physicians
- Caregivers who want to know the science supporting cognitive rehabilitation
- All rehabilitation professionals striving to deliver the latest evidence-based interventions in cognitive rehabilitation

Hans Diehl, DrHSDc, MPH, FACN
EVIDENCE-BASED RESEARCH FOR PREVENTING AND REVERSING VASCULAR DISEASES
Tue & Wed // 7 – 8 OCTOBER
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Hans Diehl, DrHSDc, MPH, FACN, Lifestyle Medicine Institute, Loma Linda, CA; Michael Greger, MD, Humane Society of the United States and Humane Society International, Washington, DC; David J.A. Jenkins, MD, PhD, DSc, University of Toronto, Toronto, ON, Canada; Robert A. Vogel, MD, Pritikin Longevity Center, Miami, FL; R. James Barnard, PhD, Pritikin Longevity Center, Miami, FL; Elizabeth Frates, MD, Institute of Lifestyle Medicine; Wayne Dysinger, MD, MPH, Lifestyle Medicine Institute, Loma Linda University, Loma Linda, CA; Heather Javaherian, OTD, Loma Linda University, Loma Linda, CA
For rehabilitation and non-rehabilitation patients, this program may assist in prevention as well as initiate the reversal process of common vascular disease. For example, vascular disease in patients with a spinal cord injury is the number one cause of death. Vascular complications can be delayed if not avoided and even reversed by providing insight, knowledge, and motivation of how patients with spinal cord injury through a better dietary lifestyle can modify their comorbidities such as overweight, hypertension, depression, and hypercholesterolemia. Further, through intensive education and a better dietary lifestyle, stroke patients can learn to address their blood pressure, reduce recurrence risk and further deterioration. READ MORE >>>
ONE-DAY COURSES // WED // 8 OCTOBER
 |
 |
 |
EARLY CAREER DEVELOPMENT COURSE
WED // 8:00 AM – 5:00 PM
OUTSTANDING VALUE from $95 USD
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
The Early Career Development Course is a perennial favorite developed by the ACRM Early Career Networking Group. It provides an ideal venue for connecting with seasoned professionals who can answer your questions and guide you on your path to success.
With particular focus on career development issues relevant to early career researchers, this full-day program will comprise a combination of didactic presentation, panel discussion, one-on-one networking, and small group discussions.
This year’s course, Charting, Navigating, or Staying Your Career Course: Identifying and solidifying your role on a team, will focus on developing and maintaining the essential skills to succeed in a team science environment.
Keynote Speaker
 We are excited to open the course with keynote speaker, Tamara Bushnik, PhD, FACRM, presenting Answering the Needs of People Requiring Rehabilitation: A National Plan to Foster Collaborative Rehabilitation Research
We are excited to open the course with keynote speaker, Tamara Bushnik, PhD, FACRM, presenting Answering the Needs of People Requiring Rehabilitation: A National Plan to Foster Collaborative Rehabilitation Research
Dr. Bushnik is Past President of ACRM, having served from October 2011 until November 2013. She has been the director of rehabilitation research at the Rusk Institute of Rehabilitation Medicine at New York University Langone School of Medicine since August 2009. Dr. Bushnik held the same position at Santa Clara Valley Medical Center from February 1999 through her move to New York City. Her research focus is firmly in the realm of post-acute recovery following acquired brain injury with a particular emphasis on the underlying mechanisms creating the common debilitation sequelae of fatigue, sleep problems and decreased community participation.
The keynote speech will be followed by an interactive panel of experts, sharing tips and tricks on leadership styles and team building. Our morning will conclude with a networking lunch designed to continue the conversations started within the earlier sessions in a more relaxed atmosphere.
Afternoon Presentations & Breakout Sessions
The afternoon will kick off with quick back-to-back “news you can use” presentations from leading funding agency representatives followed by an open question and answer panel for attendees to ask our guests the funding questions most important to you. The afternoon will continue with a panel of successful Early Career Awardees who will share their experiences obtaining funding in this competitive funding climate.
The day will culminate with two 60 minute breakout sessions, led by leaders in the field, offering multiple course options including:
- Developing Clinical/Research Teams
- Conducting Team Science
- Approaches to Team Writing
- Building a Mentorship Team
- Creating International Collaborations
- Leading/Managing a Team: What to look for when hiring
Please note: CME/CEU credit is not available for this course.
Who Should Attend?
The course is open to anyone, but targets an audience of early-career researchers, clinician scientists, and clinicians interested in starting a research agenda. Attendees range from graduate students nearing the completion of their degree, to postdoctoral scholars and junior faculty. Even if you have attended Early-Career Programs before, you can attend again! The course program changes every year, based on the needs expressed by previous course participants.
Faculty Highlights
Some of the people you can meet during the Early Career Course include program officers from major federal funding agencies, journal editors, investigators who have been successful in obtaining fellowships, career development and R01 grants, and many more experienced researchers ready to share their wisdom!
Evening Cocktail Reception
The day will conclude with a cocktail reception to enable course participants to continue to interact with each other as well as the mentors, breakout facilitators, course organizers, ACRM interdisciplinary special interest and networking group representatives, and funding-agency program officers in a relaxed, social setting.
[sm_hr]
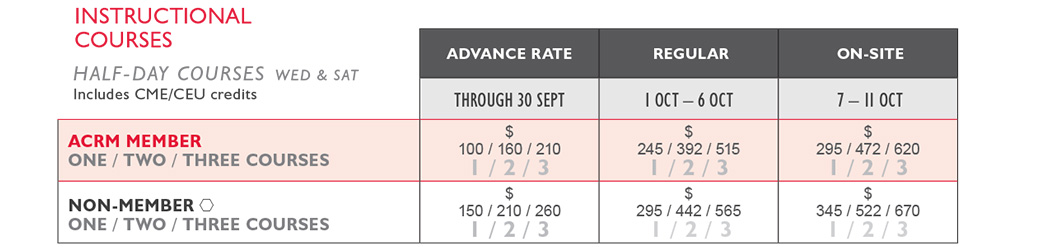
INSTRUCTIONAL COURSES
Instructional Courses are perfect for busy local clinicians, patients, their loved-ones, and researchers who want to know the latest research. Designed as intensive workshops, they provide outstanding educational value at a modest price. Continuing Education credits included for attendees’ choice of 11 disciplines.
FULL-DAY INSTRUCTIONAL COURSE
1. Coping Skills Training for Survivors of Brain Injury and Caregivers: A Workshop #1054
WED // 8:00 AM – 12:00 PM and 1:00 PM – 5:00 PM
*Note: Register for this course as TWO Instructional Courses
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Samantha Backhaus, PhD, Rehabilitation Hospital of Indiana, Indianapolis, IN; Summer Ibarra, PhD, Rehabilitation Hospital of Indiana, Indianapolis, IN
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Researchers
Emotional challenges are often present in survivors of brain injury (BI) and their caregivers. These challenges affect the person’s long-term outcomes. In this workshop, participants will learn how to facilitate an evidenced-based treatment that teaches coping skills. The morning session will be didactic, focusing on what research shows about this treatment, and the 7 Modules of this treatment. By the end of this portion, participants will acquire knowledge on what specific interventions can be provided. The afternoon session will be experiential, focusing on practicing specialized psychological techniques, and facilitating group interventions using break-out sessions.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Familiarize oneself with various modules or content areas used in this intervention
- Describe cognitive-behavioral and dialectical-behavioral strategies adapted to individuals with BI
- Discuss guidelines for facilitating the group therapy
- Acquire skills to conduct various coping skills training in small group settings
HALF-DAY INSTRUCTIONAL COURSES // WED // 8 OCTOBER
MORNING SESSIONS
2. Fatigue in Traumatic Brain Injury: Current State of Knowledge and Future Direction #1049
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Angela Colantonio, PhD, University of Toronto, Toronto, ON, Canada; Colin M. Shapiro, PhD, FRCPC, Toronto Western Hospital-UHN, Toronto, ON, Canada; Tetyana Kendzerska, MD, PhD (C), University of Toronto, Mississauga, ON, Canada; Catherine Wiseman-Hakes, PhD, Holland Bloorview Kids Rehabilitation Hospital, Toronto, ON, Canada; Tatyana Mollayeva, MD, PhD (C), University of Toronto, Toronto, ON, Canada
Diagnosis/Area of Practice: Brain Injury
Also relevant to Sleep, Preventive Medicine, Rehabilitation, Neuroscience, Occupational Medicine, Cognitive Science, Policy and Evaluation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Researchers and clinicians
This instructional course will cover a range of topics, including identification, assessment and treatment of fatigue based on current knowledge of its underlying pathophysiological pathways. Each presentation will end with a discussion, which will allow for potential formation of international collaborations and networks between rehabilitation, sleep, and TBI researchers.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Define post-traumatic fatigue (PTF)
- Provide an overview of the multifactorial etiology of PTF and be able to distinguish between fatigue, daytime sleepiness and impaired alertness
- Recognize the role of the disruption in the neuroanatomical structures which can result in impaired alertness
- Discuss appropriate methods for the assessment of fatigue in TBI practice to enhance patient outcomes and reduce potential treatment errors
- Understand current pharmacological and non-pharmacological interventions for PTF
3. Evidence, Expertise and Applicability: Key Lessons in Development and Implementation of TBI Clinical Practice Guidelines #1073
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Mark Theodore Bayley, MD, FRCPC; UHN Toronto Rehab, University of Toronto, Toronto, ON, Canada; Shawn Marshall, MD, MSc, FRCPC, Ottawa Hospital Research Institute, Ottawa, ON, Canada; Corinne Kagan, BA, BPS Cert, Ontario Neurotrauma Foundation, Toronto, ON, Canada; Isabelle Gagnon, PT, PhD, Montreal Children’s Hospital, Montreal, QC, Canada; Donna Ouchterlony, MD, St. Michael’s Hospital, Toronto, ON, Canada; Diana Velikonja, PhD, C.Psych, Hamilton Health Sciences and McMaster University, Hamilton, ON, Canada; Carol Ann DeMatteo, OT, MSc, McMaster University, Hamilton, ON, Canada; Marie-Eve Lamontagne, PhD, CIRRIS, Québec, QC, Canada; David Caplan, Ontario Neurotrauma Foundation, Toronto, ON, Canada; Robert William Teasell, MD, FRCPC, St. Joseph’s Health Care London, London, ON, Canada; Catherine Truchon, PhD, Msc Adm, Institut national d’excellence en santé et services sociaux (INESSS), Québec, QC, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians, researchers, administrators, and CPG developers
Ontario Neurotrauma Foundation and partners have developed expertise in development and implementation of clinical practice guidelines (CPGs) for rehabilitation of adult and pediatric TBI populations. This course will provide an overview of approaches taken, following established methods of gathering and analyzing evidence, evaluating quality of existing guidelines, and engaging multidisciplinary stakeholders in assessing and structuring recommendations for improved practice. Ensuring applicability for users, facilitating uptake, and balancing existing evidence with clinical realities will be addressed. Examples will be given from several initiatives across the spectrum of development and implementation from concussion/mild TBI to moderate and severe TBI.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe strategies to include and engage users in the development of clinical practice guidelines
- Discuss the roles that evidence, expert opinion and feasibility issues play in building recommendations
- Understand lessons from several approaches in knowledge translation that worked and those that did not
- Understand the facilitators and barriers to implementation and the influence of these on success
4. Getting Fit and Staying Active: Promoting Long-Term Health and Fitness in the SCI Community #1072
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Nicholas Evans, MHS, ACSM-CES, ACSM-HFS, Shepherd Center, Atlanta, GA; Mark S. Nash, PhD, FACSM, University of Miami Miller School of Medicine, Miami, FL; Audrey Hicks, PhD, McMaster University, Hamilton, ON, Canada; Jennifer French, MBA, Neurotech Network, Tampa, FL; Rachel Cowan, PhD, ACSM-CES, University of Miami, Miami, FL; Scott Bickel, PT, PhD, FACSM, University of Alabama at Birmingham, Birmingham, AL; Eric Harness, CSCS, Project Walk, Carlsbad, CA; Elizabeth Sasso, DPT, Shepherd Center, Atlanta, GA
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians: Physical Therapist (Physiotherapists), Clinical Exercise Physiologists, SCI Researchers, Certified Special Populations Trainers, Physicians
Secondary health complications are prevalent among those with disabilities and include obesity, cardiovascular disease, pulmonary disorders, and diabetes. Health care professionals must identify existing problems, diagnose relevant issues, and prescribe solutions to health concerns associated with chronic disabilities. This course will review the current health status and risks associated with spinal cord injuries. A panel of experts in SCI research and rehabilitation will provide evidenced-based recommendations for exercise prescription and programming. This will be discussed in the context of promoting healthy lifestyles throughout the continuum of care and developing innovative approaches to promoting exercise participation and adherence across the lifespan.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify the long-term health status and prevalence of secondary complications among those living with spinal cord injuries.
- Discuss the existing exercise prescription guidelines for the SCI community and explore successful approaches to implementation and information dissemination across the continuum of care.
- Identify innovative strategies for exercise promotion including the use of technology and web-based resources to reach a diverse population.
- Create and implement exercise programs to motivate initiation and continuation of participation among the SCI community.
5. Functional Electrical Stimulation for Gait: A Clinical Update in Neurorehabilitation #1171
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Michael W. O’Dell, MD, New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; Kari Dunning, PhD, College of Medicine, University of Cincinnati, Cincinnati, OH; Keith McBride, DPT, Bioness, Inc., Valencia, CA; Candy Tefertiller, MPT, ATP, NCS, Craig Hospital, Denver, CO
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
This course will provide an update on recent evidence examining the clinical effects of functional electrical stimulation on recovery and gait in persons with stroke, multiple sclerosis, and spinal cord injury. The speakers will address various aspects of FES, including its physiological basis, orthotic versus therapeutic effects, and evidence for clinical effectiveness.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the effects of lower extremity functional electrical stimulation on the peripheral and central nervous systems
- Outline recent clinical evidence for the effectiveness of FES to enhance gait in persons with selected neurological disease and injury.
- Distinguish an orthotic versus a therapeutic effect of FES on gait in persons with neurological disease and injury.
6. Multimorbidity and Secondary Health Conditions after SCI: Critical insights and Advances from the North #1517
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
José Zariffa, PhD, Toronto Rehabilitation Institute, Toronto, ON, Canada; Paul Yoo, PhD, Institute of Biomaterials and Biomedical Engineering, University of Toronto, Toronto, ON, Canada; Mohamad Sawan, PhD, École Polytechnique, Montreal, QC, Canada; Magdy Hassouna, MD, PhD, FRCSC, FACS, Toronto Western Hospital, Toronto, ON, Canada; Sukhvinder KalsiRyan, BScPT, MSc, PhD, Toronto Western Hospital, Toronto, ON, Canada; Naaz Desai, MS Rehabilitation Science, Toronto Rehabilitation Institute, Toronto, ON, Canada; B. Catherine Craven, BA, MD, FRCPC, MSc, Toronto Rehabilitation Institute, Toronto, ON, Canada; Pamela Houghton, PT, PhD, Western University, London, ON, Canada; Lora Giangregorio, PhD, University of Waterloo, Waterloo, ON, Canada
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Researchers and clinicians
Spinal cord injury (SCI) results in diverse motor, sensory, and autonomic impairments which materially contribute to the observed multimorbidity among those aging with SCI. This instructional course will be structured around three themes reflecting different aspects of managing multimorbidity after SCI: (1) Treatment of neurogenic bladder dysfunction, (2) Understanding and facilitating neurorecovery through assessment of upper limb function, and (3) Understanding the linkage between body composition and multimorbidity. Participants will have the opportunity to explore advances in technology, assessment, and the pathophysiology of multimorbidity after SCI. The course format is intended to facilitate critical thinking, hands-on learning, and small group discussions.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- To describe and critically evaluate evolving techniques to treat neurogenic bladder dysfunction after SCI
- To assist clinicians and researchers in selecting the most appropriate methods to assess and monitor
- upper limb function/recovery in the sub-acute phase after SCI
- To understand the relationships between altered body composition and health status after spinal cord injury
7. The Role of Physical Therapy Across the Patient Care Continuum in Pediatric Oncology #1385
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Susan Miale, PT, DPT, PCS, Stony Brook University, Stony Brook, NY; Raymond McKenna, PT, PhD, Stony Brook University. Stony Brook, NY
Diagnosis/Area of Practice: Cancer rehabilitation. Also relevant to pediatrics.
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
Physical therapy plays an important role in improving and maintaining the functional abilities and quality of life of children with cancer across the continuum of care, from diagnosis to survivorship. This course will highlight physical therapy and wellness interventions for children with cancer across various settings and stages of disease.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Demonstrate a basic knowledge of how to effectively screen patients to determine the need for physical therapy services in the acute pediatric oncology setting
- Identify various treatment techniques employed by pediatric physical therapists to treat children with cancer and recognize the benefits of physical therapy intervention from an evidence-based perspective
- Recognize the value of physical therapy intervention in palliative care
- Identify the role of wellness for the pediatric cancer survivor and recognize the benefits of family inclusion in wellness programs
- Identify strategies to maximize participation in physical therapy intervention and wellness programs for all participants
8. Cancer Rehabilitation: An Update and Discussion of Future Care #1055
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Julie K. Silver, MD, Harvard Medical School, Foxborough, MA; Vishwa Raj, MD, Carolinas Rehabilitation, Charlotte, NC; Nicole L. Stout, DPT, Independent consultant, Damascus, MD
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
Cancer treatment ideally involves interdisciplinary rehabilitation care. This care that is part of the continuum for other serious illnesses and injuries – such as stroke or traumatic brain injury – is often poorly implemented or entirely missing from cancer care. It is important to consider the multifaceted needs of this population including functional, psychosocial, cognitive and physical issues. This course will cover the current state of cancer rehabilitation along with the evidence base to support interventions throughout the continuum of care. Additionally, emerging issues in cancer rehabilitation care, including research needs, national and international guidelines, and recommendations will be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify the key recommendations from three important reports from the Institute of Medicine
- Cite barriers to implementing cancer rehabilitation care
- List the steps needed to develop an interdisciplinary cancer survivorship team that includes cancer rehabilitation
- Identify evidence to support cancer rehabilitation clinical interventions in various care settings
- Identify the gaps in research and recognize areas of practice where research trials would be beneficial
9. An Introduction to Longitudinal Data Analysis Part I: Continuous Outcomes #1048
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Christopher R. Pretz, PhD, Craig Hospital / NDSC, Englewood, CO; Allan John Kozlowski, PhD, Icahn School of Medicine at Mount Sinai, New York, NY; Kristen Dams-O’Connor, PhD, Mount Sinai School of Medicine, New York, NY
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Intended Audience: Researchers and clinicians
As the maturation of longitudinal datasets in rehabilitation (e.g., the SCI National Dataset and the TBI Model Systems National Dataset) continues, the need for rehabilitation researchers to appropriately assess how outcomes progress over time grows. Fortunately, a number of advanced statistical methodologies are available to accurately assess longitudinal data in the presence of continuous outcomes. Topics to be discussed include but are not limited to profile analysis, trend analysis, and linear and non-linear individual growth curve analysis. The course expands upon previously offered instructional courses in that an introduction to utilizing different software packages will be included in the agenda.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the different types of longitudinal analyses as related to continuous outcomes
- Become familiar with the different software packages used in conducting longitudinal analysis
- Properly design/conduct his/her own longitudinal research study
- Effectively communicate with statisticians/biostatisticians and other researches with respect to longitudinal analysis of continuous outcomes
- Understand the unique characteristics of longitudinal data and how these unique characteristics are accounted for in the analytic process
10. Harmonizing the Measurement of Function: From the Acute Hospital Throughout Post-Acute Care #1156
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Paulette Niewczyk, MPH, PhD, UDSMR and Daemen College, Amherst, NY; Pamela Roberts, PhD, MSHA, OTR/L, Cedars-Sinai Medical Center, Los Angeles, CA; Jacquline Mix, MS, Researcher, UDSMR, Amherst, NY; Robert Rondinelli, MD, PhD, UnityPoint Health, Des Moines, IA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians, including physicians, nurses, therapists, discharge planners as well as researchers and hospital/clinic administrators
With the possibility of bundled payment, and the establishment of accountable care organizations, assessing patients using the same measurements throughout the care continuum is crucial. This session uses ‘burden of care’ as the metric to document functional status throughout the care continuum to aid in discharge planning and document outcomes of care. This session will explain how to measure functional status and outcomes of care, and assess patient burden of care in the acute care hospital and post-acute care, including inpatient rehabilitation, skilled nursing, long-term care, home health and outpatient rehabilitation. The results of several research studies will be presented.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Define the concepts of patient burden of care and measurement of function and recognize the importance of a common outcome assessment metric used throughout the continuum of care
- Explain how to measure functional status, monitor outcomes of care, and assess patient burden of care in the acute care hospital and in post-acute care facilities, including inpatient rehabilitation, skilled nursing facilities, long-term care hospitals, home health and outpatient rehabilitation
- Describe results of research projects currently underway that incorporate the functional assessment instruments in various venues of care
11. Everything You Wanted to Know About 2014 CARF Standards and Process and Much More! #1469
Wednesday, 8 OCT // 8:00 AM – 12:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Chris MacDonell, CARF International, Washington, DC
Diagnosis/Area of Practice: Cross-cutting
Focus: Other
Intended Audience: Clinicians, administrators, quality directors, lead accreditation personnel
This session will focus on introducing CARF and its accreditation process with statistics from the most recent organizational information and address changes in the 2014 CARF Medical Rehabilitation Standards manual being used on all surveys from July 1, 2014 through June 30, 2015. Techniques to imbed standards into day-to-day practice to decrease anxiety and expense in the survey process, and tips from surveyors about preparation and review of problem areas in standards across medical rehabilitation programs will be discussed with an emphasis on problem solving and getting your questions answered.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify changes in 2014 CARF Standards manual and how they will impact your organization
- Examine different preparation techniques and utilization of standards approaches to determine best fit with your organization
- Question person-centered practices in your organization and determine if change, education, and/or dialogue is needed to ensure quality
HALF-DAY INSTRUCTIONAL COURSES // WED // 8 OCTOBER
AFTERNOON SESSIONS
12. Inter-Professional Clinical Practice Guideline for Vocational Evaluation Following Traumatic Brain Injury: Development, Implementation and Evaluation #1079
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Mary Stergiou-Kita, PhD, University of Toronto, Toronto, ON, Canada; Christina Dillahunt-Aspillaga, PhD, University of South Florida, Tampa, FL
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians, consumers, educators and program managers
This course will provide participants with an in-depth review of key research evidence relevant to return to work evaluation and planning following traumatic brain injury, training in the use of the Inter-Professional Guideline for Vocational Evaluation Following Traumatic Brain Injury and address issues related to knowledge translation and implementation.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Introduce participants to the guideline
- Train participants on how to use the guideline
- Explore how participants currently identify the key processes and factors relevant to consider within their vocational evaluations and discuss how their current clinical practices compare to the best practice recommendations
- Discuss results from pilot studies completed at two study sites, one in Toronto and one in Florida, investigating vocational evaluation practices in relation to best practice recommendations
- Identify potential facilitators and barriers to the guideline’s implementation based on evidence from pilot studies completed to date and participants’ discussions of their own practice processes
13. A Canadian Brain Injury Rehabilitation Centre for Leadership: Current and Future Directions # 1085
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Peter Rumney, MD, FRCPC; Michelle Keightley, PhD; Nick Reed, PhD, OT Reg (Ont); Ryan Hung, MSC, MD; Dayna Greenspoon, OT; Holland Bloorview Kids Rehabilitation Hospital, University of Toronto, Toronto, ON, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Pediatric Rehabilitation
Intended Audience: Clinicians
Key clinician scientists from the new Centre for Excellence in Paediatric Brain Injury Rehabilitation at the Holland Bloorview Kids Rehabilitation Hospital, University of Toronto, will present their research and best practice recommendations. Presenters include: Dr. Keightley on the structuring of active rehabilitation along with cognitive rest post-concussion; Dr. Reed with a new Constraint Induced Movement Therapy program in children with hemiparesis post-ABI; Dr. Hung on the commonality of sleep disorders in children post-ABI and their treatments; and Dr. Rumney on the reliability of the KOSCHI with an algorithm to improve the consistency of the KOSCHI scoring.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understanding of the current best practise in Paediatric Mild TBI rehabilitation and improving outcomes
- Using current tools in best practice for Outcome Assessment after Paediatric ABI at all levels of severity
- Critical evaluation of the use of CIMT in hemiparesis in children post-ABI and current models of treatment
- Approaching sleep disorders post-ABI in children from an objective and best practice approach
14. Advanced Symposium on Teaching the International Standards for Neurological Classification of Spinal Cord Injury #1096
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Ronald K. Reeves, MD, Mayo Clinic College of Medicine, Rochester, MN; Mary Schmidt-Read, PT, DPT, MA, Magee Rehabilitation, Philadelphia, PA; Members of the American Spinal Injury Association Education Committee; Candy Tefertiller, PT, DPT, ATP, NCS, Craig Hospital, Englewood, CO; Anthony Burns, MD, MSc, Toronto Rehabilitation Institute – UHN, Toronto, ON
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians with experience performing and teaching the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)
This course was developed by the American Spinal Injury Association Education Committee. It is designed for clinicians with experience performing and teaching the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) addresses: (1) challenging cases involving spinal cord injury level, severity and classification, (2) educational strategies to teach the SCI examination to new learners, and (3) how to approach some of the challenging aspects of the examination.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Determine the level, severity and completeness of even the most atypical SCI cases
- Utilize a variety of teaching strategies to meet the needs of a wide range of learning styles and objectives
- Demonstrate examination skills for the most challenging and atypical SCI situations
15. Mental Practice for Movement After Stroke: An Instructional Course for Clinicians #1229
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Stephen Page, PhD, MS, MOT, OTR/L, FAHA, The Ohio State University, Columbus, OH
Diagnosis/Area of Practice: Stroke
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
Stroke remains a leading cause of disability, with stroke induced hemiparesis remaining a primary reason for the disability exhibited by survivors. Mental practice is a noninvasive, easy to use, clinically practical approach shown to significantly reduce affected limb impairment. This course describes the theory, evidence, and clinical application of this technique in people with stroke. Attendees will also learn the outcome measures that are commonly used to optimally measure efficacy and monitor progress.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the inclusion criteria that a patient must meet to benefit from mental practice and action observation
- Describe and apply outcome measures to measure mental practice and action observation efficacy in stroke patients
- Describe the clinical protocols that should be followed to optimize efficacy of mental practice and action observation
23. An Overview of Pediatric Multiple Sclerosis
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Maria C. Milazzo, RN, MS; Moyra Rondon, LCSW
Diagnosis/Area of Practice: Neurodegenerative Diseases
Focus: Clinical Practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
Multiple Sclerosis (MS) is a common CNS disorder affecting young adults. However, nearly 5% of patients are diagnosed before age 18. Pediatric MS has evolved as a new sub-specialty as diagnostic tools have improved early diagnosis of this disease. Similar to adults, the pediatric MS population can experience difficulty with strength, balance, coordination, vision, cognition, mood, and fatigue. Affected youth and families struggle with additional challenges of an unusual and unpredictable disease, with many “hidden symptoms.” This session will provide an overview of pediatric MS, including epidemiology, diagnosis, treatment, the psychosocial impact and issues surrounding transition into adulthood with MS.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe pediatric onset multiple sclerosis
- Report the cognitive, psychosocial, and fine motor implications of pediatric multiple sclerosis
- Explain a brief evaluation battery that can be used in the clinical setting when assessing the motor skills of children with MS
- Discuss interventions for school programs and the barriers for accessing supportive accommodations in school
- Explore implications for further study
16. Cancer Rehabilitation: Utilization of Inpatient Rehabilitation for the Oncology Patient #1084
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Vishwa S. Raj, MD, Carolinas Rehabilitation, Charlotte, NC; Adrian Cristian, MD, Kingsbrook Rehabilitation Institute, Brooklyn, NY; Eugene Chang, MD, Toronto Rehabilitation Institute, University of Toronto, Toronto, ON, Canada; David Harvey, MD, Juravinski Hospital, McMaster University,Hamilton, ON, Canada
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Other or N/A
Intended Audience: Researchers, Clinicians, and Administrators
The purpose of this instructional course is to review the relevant clinical and legislative issues (both in Canada and the United States) that are relevant to the growth and development of inpatient cancer rehabilitation programs. The evidence basis for inpatient rehabilitation continues to grow, but several variables must be considered when initiating a program to maintain patient safety. In addition, different systems of practice are directly impacted by regional legislative and regulatory policies. Hence the delivery of care may vary according to diagnosis, resources available to the inpatient rehabilitation facility, and geographic location of the rehabilitation unit.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Outline the evidence basis regarding the benefits of inpatient rehabilitation for cancer patients
- Review how patient safety impacts the delivery of rehabilitation services
- Understand how rehabilitation programs may be adapted to account for diagnoses and locally available resources
- Examine how the legislative and regulatory environment for inpatient rehabilitation can affect delivery of care for oncology patients both in Canada and the United States
17. An Introduction to Longitudinal Data Analysis Part II: Non-Continuous Outcomes #1044
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Christopher R. Pretz, PhD, Craig Hospital / NDSC, Englewood, CO; Allan John Kozlowski, PhD, Icahn School of Medicine at Mount Sinai, New York, NY; Kristen Dams-O’Connor, PhD, Mount Sinai School of Medicine, New York, NY
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Intended Audience: Researchers and clinicians
As the maturation of longitudinal datasets in rehabilitation (e.g., the SCI National Dataset and the TBI Model Systems National Dataset) continues, the need for rehabilitation researchers to appropriately assess how outcomes progresses over time grows. A number of advanced statistical methodologies are available to accurately assess longitudinal data in the presence of non-continuous outcomes i.e., dichotomous/count data etc. Rehabilitation researchers will be advantageously positioned to explore a wide variety of hypotheses regarding temporal effects for observational and randomized study designs. Topics include generalized estimating equations, generalized linear mixed models, and application of individual growth curve analysis to probability of event data.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the different types of longitudinal analyses as related to non-continuous outcomes
- Become familiar with the different software packages used in conducting longitudinal analysis
- Properly design/conduct/interpret his/her own longitudinal research study
- Effectively communicate with statisticians/biostatisticians and other researches with respect to longitudinal analysis of non-continuous outcomes
- Understand the unique characteristics of longitudinal data and how these unique characteristics are accounted for in the analytic process
18. Solving Business and Clinical Dilemmas While Retaining Quality #1474
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Gary Ulicny, PhD, President/CEO, Shepherd Center, Atlanta, GA; Christopher Szybbo, President/CEO, CBI Health Group, Toronto, ON, Canada; Toril Dale, Director of Innovation and Networks, National Center for Occupational Rehabilitation, Rauland, Norway; Michael Choo, MD, Chief Medical Officer, Paradigm Management Services, Concord, CA; Michael Weinstein, MD, Medical Director, Inpatient Medical Rehabilitation Program, Eisenhower Medical Centre, Rancho Mirage, CA; Amy Hayman, Managing Director Cain Brothers, Chicago, IL
Diagnosis/Area of Practice: Cross-Cutting/CARF
Focus: Other
Intended Audience: CEO, COO, Administrative Directors, Clinical leads
This session will bring together leaders from different rehabilitation service delivery models and countries to identify business and clinical dilemmas they have faced and solved or failed at and how they are moving their organizations forward. Participants will be able to identify areas that they are working on and with the presenters learn about a structured way of collecting and sharing knowledge to develop and implement new practice in their organizations as well as problem solve with these experts solutions for their dilemmas.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Summarize common themes of dilemmas in both business and clinical arenas for rehabilitation providers.
- Analyze results in relationship to your dilemmas and determine potential solutions for your organization.
- Describe how knowledge based innovation could be a tool you use to develop and implement new practices in your organization.
19. Building a Research Culture in a Clinical Setting #1636
Wednesday, 8 OCT // 1:00 PM – 5:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Deborah Backus, PT, PhD, Shepherd Center, Atlanta, GA; Mark Bayley, MD, Brain and Spinal Cord Rehabilitation Program, Toronto Rehabilitation Institute, Toronto, ON, Canada; Chris MacDonell, CARF, Washington, DC
Diagnosis/Area of Practice: Cross-Cutting/CARF
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians, researchers and administrators in both environments, particularly those in CARF accredited institutions
An encouraging and supportive environment is an essential component for successful engagement of clinicians in both evidence-based practice and research activities. While colleges and universities have well-developed infrastructures to facilitate research processes and nurture novice researchers, clinical settings that are not part of traditional academic departments face several challenges in cultivating a research culture. Organizations, clinicians, and the people they serve, can benefit from a clinical culture that supports practitioners’ evidence-based practice and participation in research. The goal of this session is to provide strategies to transcend these challenges in order to successfully cultivate strong research cultures in clinical settings.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify the benefits of and barriers to establishing and cultivating a strong research culture in a clinical setting.
- Identify potential environments and opportunities in which clinician-researchers can attain research education and experience.
- Understand potential models to help mentor clinician-researchers to help them attain research goals.
- Understand potential opportunities and models for managers to support and facilitate clinicians’ research activities, and potential models for securing time and resources to support research activities.
- Discuss strategies for improving clinical setting infrastructures to better support clinical research activities.
HALF-DAY INSTRUCTIONAL COURSES // SAT // 11 OCTOBER
MID-DAY SESSIONS
20. A Multidisciplinary Approach in the Management of Sports Concussion #1078
Saturday, 11 October // 10:00 AM – 2:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Angela Yi, PhD; Tricia Kasamatsu, MA, ATC, Certified Athletic Trainer; Vernon Williams, MD; Jose Posas, MD; Sports Concussion Institute, Anaheim, CA
Diagnosis/Area of Practice: Brain Injury. Also relevant to pain rehabilitation.
Focus: Clinical Practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
Traumatic brain injuries sustained in sports have received increased nationwide public attention and there is a growing need for clinicians to be trained in the management of sports concussions. A sports related concussion can result in physical, cognitive, and emotional symptoms and requires a multidisciplinary network of healthcare providers who understand the various facets of sports concussion management that include prevention, assessment, diagnosis, intervention, follow-up care, and education. This instructional course will provide an overview of sports concussion management that will translate evidence and consensus-based guidelines into clinical practice and incorporate a multidisciplinary team approach to managing sports concussion.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Learn foundational information regarding the epidemiology, pathophysiology, and symptoms, of a sports related concussion
- Receive an overview of the various components that comprises a comprehensive sports concussion management program
- Understand the various roles members of a multi-disciplinary team would serve in managing a sport related concussion and post-concussion syndrome
- Explore the role of telemedicine in the delivery of sports concussion management
21. Physician Investigator Basic Training
Saturday, 11 October // 10:00 AM – 2:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Ismari Clesson, RN, Shepherd Center, Atlanta, GA; Sue Ann Sisto, PT, MA, PhD, FACRM, Stony Brook University, Stony Brook, NY; Flora Hammond, MD, Indiana University, Rehabilitation Hospital of Indiana, Indianapolis, IN; Mike Jones, PhD, Shepherd Center, Atlanta, GA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Intended Audience: Physicians, nurses, therapists, and other healthcare professionals involved in or interested in clinical research.
The purpose of this course is to assist new physician investigators and key research staff in improving their skills and understanding of the principles and practices used in the successful execution of patient-oriented research. Participants will gain insights to enhance their ability to perform qualify research according to existing regulations and guidelines. The course is open to physicians, nurses, therapists, and other healthcare professionals involved in or interested in clinical research. The program will share information and create an opportunity for dialogue amongst attendees and program faculty.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the current landscape of clinical research and opportunities for the physician investigator
- Discuss issues in the design, conduct, and management of successful clinical research studies
- Discuss investigator responsibilities related to regulations and ethics
- Describe avenues for dissemination and collaboration
22. Ensuring the Delivery of High-Quality Fall Prevention: How Rehabilitation Professionals Engage in Quality Improvement #1294
Saturday, 11 October // 10:00 AM – 2:00 PM
![]() OR Call +1.703.574.5845
OR Call +1.703.574.5845
Faculty
Natalie E. Leland PhD, OTR/L, BCG, FAOTA, University of Southern California, USC Davis School of Gerontology, Los Angeles, CA; Anne Deutsch, PhD, RTI International, Northwestern University Feinberg School of Medicine, Chicago, IL; Pamela Roberts, PhD, MSHA, OTR/L, SCFES, FAOTA, CPHQ, Cedars-Sinai Medical Center, Los Angeles, CA; Jennifer C. Sidelinker, PT, DPT, GCS, Genesis Rehab Services, Kennett Square, PA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Rehabilitation clinicians, administrators, and provider organizations engaging in quality improvement initiatives and facilitating the translation and implementation of evidence into the clinical setting.
The translation and implementation of evidence into practice and an organization’s continuous quality improvement are pivotal for reducing the occurrence of poor patient outcomes – imperative in the era of the Affordable Care Act (ACA). Using a rehabilitation relevant to the adverse event of accidental falls as an exemplar, this symposium will provide an overview of how rehabilitation professionals and administrators can collaborate in the provision of high-quality care. Evidence and practice examples will be discussed in the context of ACA value-based payment, quality improvement, and implementation science, to equip participants with tools to enhance quality improvement initiatives in their practice setting.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe current fall prevention evidence for in-hospital and post-acute care rehabilitation patients.
- Discuss the role of value-based purchasing in the context of rehabilitation service delivery.
- Identify the theoretical constructs that support the translation and implementation of evidence into practice.
- Verbalize the key components of continuous quality improvement.