Core Conference Program
[clear][spacer
COURSE DESCRIPTIONS // FRIDAY & SATURDAY (PDF)
THU, 9 OCTOBER AGENDAFRI, 10 OCTOBER AGENDASAT, 11 OCTOBER AGENDA
See the BIG picture.Program At-A-Glance >>>
|
 |
 |
<<< Click to View
|
CORE CONFERENCE RUNNING SCHEDULE
THURSDAY, 9 OCTOBER 2014
Expo Open // 10:00 AM – 7:00 PM
ACRM SPECIAL INTEREST & NETWORKING GROUP MEETINGS
Stroke-ISIG Kick-Off Meeting
THU // 7:00 AM – 8:00 AM
SCI-ISIG: Fitness and Wellness Task Force Meeting
THU // 7:00 AM – 8:00 AM
Outcomes Measurement Networking Group Meeting
THU // 7:00 AM – 8:00 AM
International Networking Group Business Meeting
THU // 7:00 AM – 8:00 AM
Early Career Networking Group: Physicians Task Force Meeting
THU // 7:00 AM – 8:00 AM
Military and Veterans Affairs Networking Group Meeting
THU // 7:00 AM – 8:00 AM
Pediatric Rehabilitation Networking Group Meeting
THU // 7:00 AM – 8:00 AM
 WELCOME REMARKS AND OPENING PLENARY SESSION
WELCOME REMARKS AND OPENING PLENARY SESSION
Pushing, Pulling, Nudging and Tipping Evidence Into Practice: Experience From the Frontline Implementing Best Practices in Rehabilitation
THU // 8:00 AM – 10:00 AM
Faculty
Mark Theodore Bayley, MD, FRCPC; UHN Toronto Rehab, University of Toronto, Toronto, ON, Canada
While there has been an increasing focus on evidence-based practice, there continue to be delays in translation of novel research into practice. Health systems research shows that many individuals receive inappropriate, unnecessary or at worst, harmful care. Current funding restraints demand that providers find faster ways to uptake new evidence and ensure that patients receive best practice care. Rehabilitation providers face additional challenges in implementing evidence- based care because of the complexity of interprofessional interventions, tailoring their treatment to the individual patient in front of them, changing treatment as recovery occurs and selecting and prioritizing treatments from many different options.
This presentation will provide an overview of an approach to implementation that involves first identifying the barriers to uptake of evidence. The presentation will then give examples of implementation strategies from projects in the field of rehabilitation.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the challenges in implementing best practices and the steps in the knowledge to action cycle
- Name 3 sources of barriers to implementation of evidence
- Discuss evidence- based strategies for implementing best practices in their own work environment using the examples provided
Dr. Bayley is medical director of the Brain & Spinal Cord Rehabilitation Program at Toronto Rehab in Toronto, Ontario, Canada, assistant professor in the faculty of medicine at the University of Toronto, and chair of the ABI Committee at the Ontario Neurotrauma Foundation.
NETWORKING BREAK // EXPO OPEN
THU // 10:00 AM – 11:00 AM
Interventions Affecting Outcomes Following Traumatic Brain Injury Rehabilitation # 1152
THU // 11:00 AM – 12:30 PM
Faculty
John D. Corrigan, PhD, Ohio Regional TBIMS, Ohio State University, Columbus, OH; Susan D. Horn, PhD, Institute for Clinical Outcomes Research, Salt Lake City, UT; Cynthia L. Beaulieu, PhD, ABPP-CN, Brooks Rehabilitation Hospital, Jacksonville, FL; Flora M. Hammond, MD, Indiana University School of Medicine, Rehabilitation Hospital of Indiana, Indianapolis, IN
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This symposium will present data from the Traumatic Brain Injury Practice-Based Evidence study of 2,130 patients who received acute, inpatient rehabilitation at 9 U.S. and 1 Canadian facility. Individual differences in patient characteristics and status upon admission to rehabilitation will be associated with the nature and extent of therapies provided and medications used. Outcomes at discharge and 9 months later will be described and associated with interventions provided during rehabilitation.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe how the TBI PBE study addresses comprehensive TBI rehabilitation care in order to determine those therapeutic and pharmacological treatments that are associated with better outcomes for specific types of patients
- Describe differences in treatments by admission FIM cognitive subgroups of patients with TBI during rehabilitation and after discharge
- Describe differences in outcomes by admission FIM cognitive subgroups of patients with TBI during rehabilitation and after discharge
- Describe treatments associated with better outcomes by admission FIM cognitive subgroups of patients at rehabilitation discharge and 1-year post-injury
Long-Term Social Role Difficulties for the Person With a Brain Injury and a Psychiatric Diagnosis #1139
THU // 11:00 AM – 12:30 PM
Faculty
Rolf B. Gainer, PhD, Neurologic Rehabilitation Institute, Brookhaven Hospital, Tulsa, OK; Paitra Surerus, MA, Neurologic Rehabilitation Institute of Ontario, Etobicoke, ON, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Individuals living with a brain injury and a psychiatric or substance abuse disorder experience significant problems in social role return and in their relationships. The social role return problem becomes a barrier to long-term reintegration into community living and may be a factor in the isolation and withdrawal of the individual. It can also contribute to further reducing the person’s ability to manage psychiatric problems such as depression, anxiety and substance abuse. A significant number of individuals experience severe disruption in their home and community and can experience a high risk for homelessness and incarceration without extended supports.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify the barriers to social role return for the person with brain injury and a “dual diagnosis”
- Examine the aspects of social network failure which may exacerbate psychiatric issues following brain injury
- Consider the significance of isolation, loneliness and social withdrawal as barriers to social role return
The World Health Organization’s (WHO) International Perspectives on Spinal Cord Injury (IPSCI) Report: Implications #1101
THU // 11:00 AM – 12:30 PM
Faculty
Yuying Chen, MD, PhD, National SCI Statistical Center, University of Alabama at Birmingham, Birmingham, AL; Anthony S. Burns, MD, MSc, University of Toronto, Toronto Rehabilitation Institute, Toronto, ON, Canada; Marcel W. M. Post, PhD, De Hoogstraat, University Medical Center, Utrecht, The Netherlands; Per Maximilian von Groote, MA, University of Lucerne and Swiss Paraplegic Research, Nottwil, Switzerland; Susan Charlifue, PhD, FACRM, Craig Hospital, Englewood, CO; Armando Vasquez Barrios, MD, Region of the Americas/World Health Organization, Buenos Aires, Venezuela
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Health/disability policy, ethics, advocacy
Goals of this ACRM symposium are to: (a) present the IPSCI report, (b) discuss core issues of the report by presenting the evidence behind the text and relating this evidence to clinical practice, and (c) to discuss how recommendations of such a WHO report can be implemented. Specific focus will be on global perspectives addressing the following areas: SCI epidemiology, meeting health care and rehabilitation needs after SCI in high- and low-resource settings, employment and evidence of barriers and facilitators to equal participation, and implementing the WHO reports bridging the gap from recommendations to evidence-informed policy and practice.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the content of the IPSCI report and its potential impact on policy and practice worldwide
- Describe differences in SCI epidemiology around the world
- Describe barriers and facilitators to employment after SCI in various countries
- Discuss differences in high- and low-resource countries in addressing rehabilitation and health needs for people with SCI
Improving Walking Ability in Patients After Stroke: Different Roads Lead to Rome #1151
THU // 11:00 AM – 12:30 PM
Faculty
Johan S. Rietman, MD, PhD, Laboratory of Biomechanical Engineering, University of Twente, Enschede, The Netherlands; Jaap Buurke, PT, PhD, Roessingh Research and Development, Enschede, The Netherlands; Corien Nikamp, MSc, Roessingh Research and Development, Enschede, The Netherlands; G.J. Bertjo Renzenbrink, MD, Sint Maartenskliniek Rehabilitation Centre, Nijmegen, The Netherlands; Martin J. B. Tenniglo, PT, Roessingh Centre for Rehabilitation, Roessingh Research and Development, Enschede, The Netherlands
Diagnosis/Area of Practice: Stroke
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Serious walking problems in stroke patients lead to impaired community ambulation and subsequently decreased quality of life. Therefore, recovery of walking ability is one of the most relevant functional targets of rehabilitation after stroke. This symposium will provide new knowledge from different research projects on the contribution of the paretic and non-paretic leg to recovery of balance control and walking, the effects of timing of providing AFOs, soft tissue surgery in equinovarus foot deformity, and functional electrostimulation of the hamstrings or chemodenervation rectus femoris in stiff knee gait.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the contribution of the paretic and non-paretic leg to balance control after stroke
- Describe functional recovery or compensation strategies in balance control after stroke
- Describe the effect of timing of AFOs on walking ability after stroke
- Understand the effect of soft-tissue surgery for equinovarus foot deformity on walking ability
- Understand the effect of hamstring stimulation in stiff knee gait
An Interdisciplinary Update on Exercise in Multiple Sclerosis: State of the Art and Practical Applications #1182
THU // 11:00 AM – 12:30 PM
Faculty
Tania R. Bruno, MD, FRCPC, CSCN Dip (EMG), FAAPMR, Toronto Rehab, UHN, University of Toronto, Toronto, ON, Canada; Amy E. Latimer-Cheung, PhD, School of Kinesiology and Health Studies, Queen’s University, Kingston, ON, Canada; Deborah Backus, PT, PhD, Eula C. and Andrew C. Carlos MS Rehabilitation and Wellness Program, Shepherd Center, Atlanta, GA; Jo-Anne Howe, DipP&OT, BScPT, Toronto Rehab, UHN, University of Toronto, Toronto, ON, Canada; Blake Burdett, ES, BScKin, Eula C. and Andrew C. Carlos MS Rehabilitation and Wellness Program, Shepherd Center, Atlanta, GA
Diagnosis/Area of Practice: Neurodegenerative disease (e.g., MS, Parkinson’s disease)
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Current research has established that adult persons with Multiple Sclerosis are able to respond physiologically to exercise. Practical applications of this research are at the forefront of rehabilitation efforts at the quaternary/tertiary care levels and are now making headway into municipal community programs as well as at patient empowerment levels. This symposium will review the current evidence for exercise in MS, discuss the direction of future necessary research endeavors, and present clinical applications at the individual as well as group levels. An interdisciplinary group of presenters will span the expertise from basic science to clinical medicine to physical therapeutics.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Recognize the role of exercise and increased physical activity in the management of persons with multiple sclerosis
- Discuss the barriers to conducting exercise-related research in this population
- Identify strategies to increase therapeutic exercise opportunities for persons with multiple sclerosis at the individual and community levels
Opioids for Chronic Non-Cancer Pain: Update on the Scientific Evidence and Practical Aspects of Prescribing #1211
THU // 11:00 AM – 12:30 PM
Faculty
Jaemin Kim, MPH, Institute for Work & Health, Toronto, ON, Canada; Andrea D. Furlan, MD, PhD, University of Toronto, Toronto, ON, Canada; John Flannery, MD, FRCPC, University of Toronto, Toronto, ON, Canada; Sivakumar Gulasingam, MD, University of Toronto, Toronto, ON, Canada; Emma Irvin, BA, Institute for Work & Health, Toronto, ON, Canada; Dwayne Van Erd, MSc, PhD (c), Institute for Work & Health, Toronto, ON, Canada; Nancy Carnide, PhD (c), Institute for Work & Health; Claire Munhall, MPH, Institute for Work & Health, Toronto, ON, Canada; Melanie Fortune, MPH, Institute for Work & Health, Toronto, ON, Canada
Diagnosis/Area of Practice: Pain
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Chronic non cancer pain (CNCP) is a substantial health concern in Canada and globally. Opioids have been used for treatment of CNCP because of their potent analgesic nature. Adverse effects and abuse due to its long-term use have been reported in many journals and literatures. This symposium is intended to enhance the knowledge and comfort of clinicians and researchers involved in the care of those with CNCP and opioid prescription. This includes synthesis of the latest scientific literature, evidence-based measures, impact of long-term therapy, effective tools to aid opioid therapy, and conversation strategies around opioid prescription.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the scientific evidence of opioids in the treatment of chronic non-cancer pain
- Discuss how to conduct an N-of-1 Trial of opioid for chronic non-cancer pain
- Demonstrate knowledge and practice skills to say “No” when encountered with inappropriate requests for opioids
Advancing Cancer Survivorship Care With Integrated Cancer Rehabilitation Treatment Algorithms for Symptom Management #1246
THU // 11:00 AM – 12:30 PM
Faculty
W. Christian VandenBerg, MD; Mary Free Bed Rehabilitation Hospital (MFBRH), Michigan State University, Grand Rapids, MI; Lorraine J. Pearl-Kraus, PhD, CS, FNP-BC, Mary Free Bed Rehabilitation Hospital, Grand Rapids, MI
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Delayed and long-term side effects of cancer and cancer-related treatments impact cancer survivors’ functionality and quality of life. Chemotherapy-induced peripheral neuropathies and mild cognitive impairment (chemobrain) are common sequelae cancer survivors experience. This symposium will provide an overview of development of a prospective surveillance, integrated cancer rehabilitation care model and treatment algorithms designed to: (a) optimize functionality and quality of life and (b) improve care outcomes of cancer survivors who experience CIPN and/or mild cognitive impairment (chemobrain) due to their cancer and its related treatments.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the processes involved in establishing collaborative relationships with oncology colleagues
- Explain how the prospective surveillance model is applied to cancer symptom management
- Explain the Chemotherapy-induced Peripheral Neuropathy Rehabilitation Treatment Algorithm and rationale for selected outcome measures
- Explain the Cognitive Dysfunction/Chemobrain Treatment Algorithm and rationale for selected outcome measures
- Discuss the impact of health system fragmentation and identified barriers to cancer survivorship care
Pediatric Concussion: Who, What, When, Where, and Why #1142
THU // 11:00 AM – 12:30 PM
Faculty
Stacy Suskauer, MD, Kennedy Krieger Institute, Johns Hopkins University School of Medicine, Baltimore, MD; Drew Davis, MD, University of Alabama Birmingham, Birmingham, AL; Julie Haarbauer-Krupa, PhD, National Center for Injury Preventions and Control, Centers for Disease Control and Prevention, Atlanta, GA; Amy Houtrow, MD, PhD, MPH, Rehabilitation Institute, Children’s Hospital of Pittsburgh, Pittsburgh, PA; Brad Kurowski, MD, Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine, Cincinnati, OH
Diagnosis/Area of Practice: Brain Injury
Focus: Pediatric Rehabilitation
There is growing evidence regarding pediatric concussion which can be used to inform clinical care. This symposium will showcase data from research efforts at multiple institutions, providing an introduction to findings relevant to the care of children with concussion. Talks will address “WHO” is incurring pediatric sports-related concussion, “WHAT” interventions appear effective for treating children who are slow to recover, “WHEN” younger children with concussion are discharged from specialty care, that “WHERE” within a health system children receive care affects consistency of care, and “WHY” health and social systems need to be optimized to meet the needs of this population.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe trends in sports related Traumatic Brain Injury in children
- Name one intervention that can be used for children with persistent post-concussive symptoms
- Describe the timeline to discharge from a specialty concussion clinic in a sample of children aged 6-12 years
- Describe the process of developing a concussion clinical care pathway across multiple medical disciplines within a large academic medical center
- Identify the economic impact of concussion in children
How to Get Published: Authorship, Reporting Guidelines, Reviewing in Medical Rehabilitation #1167
THU // 11:00 AM – 12:30 PM
Faculty
The faculty for this symposium is comprised of editors of the ACRM scientific journal, Archives of Physical Medicine and Rehabilitation, including:
Allen W. Heinemann, PhD, Rehabilitation Institute of Chicago, Chicago, IL; Leighton Chan, MD, MPH, Clinical Center, National Institutes of Health, Bethesda, MD; Helen Hoenig, MD, BS (OT), MPH, Duke University Medical Center, Durham, NC; Jeffrey R. Basford, MD, PhD, Mayo Clinic, Rochester, MN; Duncan Babbage, PhD, Auckland University of Technology, Auckland, New Zealand; Dawn M. Ehde, PhD, University of Washington School of Medicine, Seattle, WA; Amy Houtrow, MD, PhD, MPH, University of Pittsburgh, Pittsburgh, PA; Jay Meythaler, MD, JD, Wayne State University, Dearborn, MI; Elliot J. Roth, MD, Rehabilitation Institute of Chicago/Northwestern University, Chicago, IL; Janet M. Powell, PhD, OTR/L, FAOTA, University of Washington, Seattle, WA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Other
Highly recommended for all Early Career researchers, this symposium addresses issues faced by authors in preparing a manuscript for peer review, and by peer reviewers in evaluating manuscripts for publication. This symposium will cover a range of topics of interest to everyone involved in scientific publishing, including: authorship, preparing and submitting your manuscript, reporting guidelines, trial registration, reviewing manuscripts, publication ethics, open access, and digital innovations in publishing – a “must-attend” event for early career professionals. Many topics will have a general publishing focus but we will focus specifically on the ACRM scientific journal, Archives of Physical Medicine and Rehabilitation.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss issues in preparing a manuscript for peer review
- Describe reporting guidelines and methods to assure effective integration in the preparation of a research project
- Describe issues in serving as an effective peer reviewer for a scientific article
Translating Research into Person-Centered Practices in Rehabilitation: Examples From the US, Canada, and New Zealand #1192
THU // 11:00 AM – 12:30 PM
Faculty
Christina Papadimitriou, PhD, Northern Illinois University, DeKalb, IL; Pia Kontos, PhD, Toronto Rehabilitation Institute-University Health Network, Toronto, ON, Canada; Kathryn McPherson, AUT University, Auckland, New Zealand; Christine MacDonell, CARF International, Washington, DC
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This symposium will focus on three distinct populations of rehabilitation clients: those with traumatic brain injury (TBI), spinal cord injury/ dysfunction (SCI/D), or stroke. We draw from research activities conducted in three countries: Canada, the United States, and New Zealand to explore client experiences and novel developments in person-centered practice in inpatient and community rehabilitation contexts. Our goal is to identify challenges of person-centeredness and ways in which researchers have attempted to assist providers toward engaging in more person-centered ways. In our presentations we facilitate the audience’s thinking of their daily practice and how to move toward more person-centered approaches.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify and define more clearly key elements of person-centered rehabilitation practice
- Identify potential areas for improvement in one\’s organization\’s person-centered practices through self-assessment
- Explore use of three different approaches, in three different jurisdictions, each aiming to translate
Innovative Strategies to Promote Exercise Participation and Adherence Among Individuals With Mobility Impairments #1205
THU // 11:00 AM – 12:30 PM
Faculty
Mark S. Nash, PhD, FACSM, Lois Pope Life Center, University of Miami Miller School of Medicine, Miami, FL; Jennifer French, MBA, Neurotech Network, Tampa, FL; Nick Evans, MHS, ACSM-CES/HFS, Virginia C. Crawford Research Institute, Shepherd Center, Atlanta, GA; C. Scott Bickel, PT, PhD, FACSM, School of Health Professions, University of Alabama at Birmingham, Birmingham, AL
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Physical activity levels are typically low among those with mobility impairments, leading to long-term health complications. Research has demonstrated that low exercise participation is often due to unique physical, environmental, and psychosocial barriers. Health care professionals are in the ideal position to positively affect long-term health outcomes by promoting exercise throughout the continuum of care, developing effective strategies to overcome participation barriers, and encouraging healthy lifestyles. This symposium will address innovative and cost effective approaches to promoting fitness participation and exercise adherence. The session will end with a discussion of how these strategies can be applied to various diagnostic groups.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify existing exercise participation barriers and health complications among those with mobility impairments due to neurological conditions
- Explore novel strategies including the use of technology, web-based resources and innovative programming to improve health promotion to a diverse population
- Recommend strategies to translate recommendations into executable exercise programs to the mobility impaired community
The Inpatient Rehabilitation Experience of Patients With Cancer #1304
THU // 11:00 AM – 12:30 PM
Faculty
Jacqueline Mix, MPH, State University of New York at Buffalo, Uniform Data System for Medical Rehabilitation, Amherst, NY; Ki Shin, MD, University of Texas MD Anderson Cancer Center, Houston, TX
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Outcomes research/epidemiology
There is evidence that improving functional status of cancer patients leads to improved health and quality of life. Inpatient rehabilitation programs providing intensive rehabilitation therapy have been shown to improve functional status in persons with cancer, yet these programs are underutilized by this patient population. The goal of this symposium is to provide an overview of the rehabilitation needs of individuals with cancer and to discuss the unique challenges present for cancer patients in the inpatient rehabilitation setting. Results of an ongoing multi-center research study of the predictors of functional outcomes of inpatient rehabilitation among cancer patients will also be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify the rehabilitation needs of patients with cancer
- Review existing literature regarding the impact of functional status on disease prognosis in the cancer population
- Review existing literature regarding functional outcomes among cancer patients in the inpatient rehabilitation setting
- Report on and discuss results from a multi-center study of cancer patients seen in inpatient rehabilitation facilities
Oral Presentation of Scientific Papers — Brain Injury Topics
THU // 11:00 AM – 12:30 PM
Moderator: Tamara Bushnik, PhD, FACRM
11:00 – 11:20: Mortality in Individuals Unable to Follow Commands at the Time of Rehabilitation Admission (#1823)
Presented by Brian Greenwald
11:20 – 11:40: Effect of Lesion Burden on Recovery and Response to Amantadine in Patients with Traumatic Disorders of Consciousness (#1840)
Presented by Douglas Katz
11:40 – 12:00: Risk Factors Associated with Acute Rehospitalization after Inpatient Rehabilitation (#1673)
Presented by Amol Karmarkar
12:00 – 12:20: The Relationship between Sleep Architecture and Symptoms of Sleep Disturbance in Individuals with Traumatic Brain Injury (#1723)
Presented by William Lu
Brain Injury Interdisciplinary Special Interest Group (BI-ISIG) Annual Summit
THU // 12:30 PM – 1:45 PM
SCI-ISIG: Women’s Health Task Force Meeting
THU // 12:30 PM –2:00 PM
LUNCH BREAK // EXPO OPEN
12:30 PM – 2:00 PM
LUNCH PROGRAMS
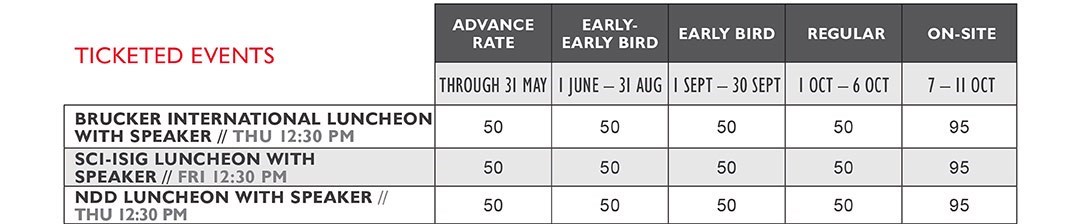
Keep learning, connecting, and earning CE credits right through lunch! Sponsored by ACRM Special Interest and Networking Groups, these onsite lunch programs feature renowned guest speakers and specialty topics and provide an ideal setting for connecting with like-minded colleagues.
Add a luncheon to your existing registration at any time by simply returning to online registration.
 NEURODEGENERATIVE DISEASES NETWORKING GROUP LUNCHEON
NEURODEGENERATIVE DISEASES NETWORKING GROUP LUNCHEON
with Speaker, Dr. John DeLuca
THU // 12:30 PM – 2:00 PM
$ Ticketed Event
![]()
Cognitive Rehabilitation in Multiple Sclerosis: A Behavioral and Neuroimaging Analysis
John DeLuca, PhD is senior vice president for research at the Kessler Foundation Research Center, a professor in the Departments of Physical Medicine & Rehabilitation (PM&R) and Neurology and Neuroscience at Rutgers New Jersey Medical School, and a licensed psychologist in the states of New Jersey and New York. He is currently studying disorders of memory and information processing in a variety of clinical populations including multiple sclerosis and traumatic brain injury. Dr. DeLuca’s accomplishments include over 275 published articles, abstracts, and chapters in these areas.
 BRUCKER INTERNATIONAL LUNCHEON
BRUCKER INTERNATIONAL LUNCHEON
with Speaker, Dr. Donald T. Stuss
THU // 12:30 PM – 2:00 PM
$ Ticketed Event
![]()
Completing the Circle Between Science and Rehabilitation: The Ontario Brain Institute Story
Effective rehabilitation might be described as the right treatment for the right person at the right time. The definition of “right” for each section is important. The “right treatment” means it is based on a theoretically driven, validated, and tested approach, which is continually updated and refined as knowledge changes. The “right person” suggests that rehabilitation needs to be directed to a well-characterized subgroup and that not all interventions might be applicable for everyone. The “right time” identifies the most efficacious opportunity. The way to achieve this is by integrating basic and clinical research, as well as patients and their advocacy groups and industry, in an open and collaborative enterprise. The presentation will outline the structure of the Ontario Brain Institute as a possible method to achieve maximum health impact.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Relate the concept of group heterogeneity (intra-group variability) to effective rehabilitation
- Identify at least three advantages of an approach to science which integrates basic and clinical research, as well as patients & industry
- Outline the basic tenets of the Ontario Brain Institute system to create Science with clinical/economic impact
Donald T. Stuss, PhD, C. Psych, ABPP-CN, Order of Ontario, FRSC, FCAHS, is the founding president and scientific director of the Ontario Brain Institute and a professor of medicine at the University of Toronto. He founded the Rotman Research Institute in 1989 and served as director until 2008. Dr. Stuss is a fellow of CPA, APA (Divisions 3, 6, 20, 40), APS, the American Heart and Stroke Association, and the AAAS, and was honored with Lifetime Achievement Awards by the NAN and INS. His research concentrates on understanding and treating the cognitive functions and personality changes associated with the frontal lobes in various disorders. He has published over 200 peer-reviewed manuscripts, 49 chapters, and one co-authored and four edited books.
Cancer Rehabilitation Networking Group Meeting
[sm_hr]
30-MINUTE SYMPOSIA SERIES
THU // 1:30 PM – 3:00 PM
Moderator: Nicole Stout, PT, DPT, CLT-LANA
A concentrated look at three topics in a single session.
1:30 PM – 2:00 PM: Mindfulness-Based Cognitive Therapy for TBI Reduces Symptoms of Depression: Results From a Randomized Controlled Trial (#1839)
Presented by Melissa Felteau, Lakehead University, Thunder Bay, ON, Canada
2:00 PM – 2:30 PM: Predicting Future Prosthetic Function: A Prognostic Screening Tool and Clinical Prediction Rule (#1175)
Faculty
Christopher Kevin Wong, PT, PhD; Christine C. Chen, Columbia University Medical Center, New York, NY
Rehabilitation for people with lower limb amputations has shifted from hospitals to the community. However, medical issues often complicate rehabilitation after amputation, even for those healthy enough for home discharge, leading to delayed prosthetic fitting and lower outcomes. While many factors can affect prosthetic outcomes, balance is the most consistent variable associated with successful prosthetic walking. This symposium presents a valid and reliable clinical balance assessment for community-dwelling people with lower limb amputation; and a clinical prediction rule to accurately determine future successful prosthetic function, derived from a short clinical screening method for use by physicians, prosthetists, and rehabilitation therapists.
Learning Objectives
- Understand how the Berg Balance Scale can be applied for community-dwelling people with lower limb amputations in a valid and reliable manner
- Describe the impact of background research on the development of the prognostic clinical prediction rule for prosthetic function
- Apply the clinical prediction rule with understanding of its prognostic accuracy for the diverse population of community dwelling people with lower limb amputation
- Perform the clinical screening method in less than 5 minutes
2:30 PM – 3:00 PM: Pediatric Spinal Cord Injury: A Family-Centered and Restorative Approach to Gait Training
Faculty
Lauren A. White, PT, DPT, PCS; Amanda Oakley, PT, DPT, International Center for Spinal Cord Injury at Kennedy Krieger Institute, Baltimore, MD
The presence of spinal cord related neurological injury has a major impact on a child’s gross motor function, access to their environment, ability to participate in age appropriate play, and quality of life. Utilizing current evidence-based intervention, we will demonstrate a clinical decision-making algorithm for gait training in the very young pediatric population, as compared to conventional habilitation models. This symposium will address clinical rationale for inclusion of technological advancements in pediatric gait training, as well as outcomes from our clinical experience that demonstrate a progressive, activity-based approach to gait training in the pediatric population is safe and effective.
Learning Objectives:
- Identify current, evidence-based strategies for gait training in young (0-5 years of age) pediatric population with spinal cord related neurological impairments
- Understand the impact of restrictive bracing on an impaired nervous system
- Demonstrate appropriate clinical rationale for the use of specific gait training interventions
[sm_hr]
SHELDON BERROL MEMORIAL CHAUTAUQUA
A CALL TO ACTION FOR HEALTH DISPARITIES
THU // 2:00 PM – 3:30 PM
FREE Ticketed Event
The Sheldon Berrol Chautauqua is the BI-ISIG special annual session where timely and sometimes controversial issues are addressed and colleagues come together to explore topics that provoke questions of values, ethics, and humanism in brain injury rehabilitation.
The 2014 Chautauqua topic, A Call to Action for Health Disparities addresses inequities of care and common issues across mechanisms of injury and injury contexts.
Moderators: Angela Colantonio, PhD and Yelena Goldin, PhD
Panelists: Halina (Lin) Haag, MSW, RSW and Heather Shepherd, BSc
Diagnosis/Area of Practice: Brain Injury
Healthcare disparities are prevalent among individuals with traumatic brain injury (TBI), especially in under-represented populations and represent a lack of efficiency within the scientific and clinical community. The current state of the science is marked by segmentation of the field of TBI in pursuit of the next “hot topic,” which is one reason these inequities persist.
This fragmentation is evident in the nomenclature and approaches across injury settings (civilian TBI, military TBI, and sports concussions) and diverts the focus from long-term effects of injury that are common among individuals with TBI, regardless of injury mechanism or venue. Bridging the gap between various settings and nomenclatures to highlight the universal needs of all individuals affected by TBI is the first step to addressing healthcare disparities perpetuated by the segmentation of the field.
At the 2014 Chautauqua, we will discuss the cross cutting experiences and functional implications of TBI among women with civilian, sports-related, and military blast injuries. Representative consumers from these diverse populations will share their experiences and perspectives on needs and disparities in medical care, behavioral care, and socioeconomic support.
Representative clinician-researchers will provide a state-of-the science context for the issues that emerge from the discussion to offer recommendations and future directions to clinicians, researchers, and consumers. Recent policy changes implemented by the National Institutes of Health with the aim of reducing inequities will be highlighted in the session.
 MODERATOR: Angela Colantonio, PhD, OTR, FACRM is a professor at the University of Toronto in the Department of Occupational Science & Occupational Therapy and a senior scientist at Toronto Rehabilitation Institute, UHN. Dr. Colantonio also holds a CIHR Research Chair in Gender, Work and Health focusing on brain injury. She received her PhD in Epidemiology and Public Health from Yale University, and an MSc in Community Health and a BSc in Occupational Therapy from the University of Toronto. She leads an internationally recognized program of research on acquired brain injury (ABI) that includes examination of ABI in the population targeting injury prevention and post-acute care with a special focus on vulnerable populations. She is the co-chair of the BI-ISIG Girls and Women with ABI Task Force.
MODERATOR: Angela Colantonio, PhD, OTR, FACRM is a professor at the University of Toronto in the Department of Occupational Science & Occupational Therapy and a senior scientist at Toronto Rehabilitation Institute, UHN. Dr. Colantonio also holds a CIHR Research Chair in Gender, Work and Health focusing on brain injury. She received her PhD in Epidemiology and Public Health from Yale University, and an MSc in Community Health and a BSc in Occupational Therapy from the University of Toronto. She leads an internationally recognized program of research on acquired brain injury (ABI) that includes examination of ABI in the population targeting injury prevention and post-acute care with a special focus on vulnerable populations. She is the co-chair of the BI-ISIG Girls and Women with ABI Task Force.
 MODERATOR: Yelena Goldin, PhD is a fellowship-trained clinical and research neuropsychologist at the JFK-Johnson Rehabilitation Center and a clinical assistant professor of Physical Medicine and Rehabilitation at Rutgers University Robert Wood Johnson Medical School. She is the co-chair of the BI-ISIG Girls and Women with ABI Task Force. Her research focuses on conducting clinical and basic research addressing outcomes of injury and rehabilitation with individuals with TBI. Her clinical work in neuropsychology and cognitive rehabilitation focuses primarily on acquired brain injury.
MODERATOR: Yelena Goldin, PhD is a fellowship-trained clinical and research neuropsychologist at the JFK-Johnson Rehabilitation Center and a clinical assistant professor of Physical Medicine and Rehabilitation at Rutgers University Robert Wood Johnson Medical School. She is the co-chair of the BI-ISIG Girls and Women with ABI Task Force. Her research focuses on conducting clinical and basic research addressing outcomes of injury and rehabilitation with individuals with TBI. Her clinical work in neuropsychology and cognitive rehabilitation focuses primarily on acquired brain injury.
 PANELIST: Halina (Lin) Haag, MSW, RSW is a Canadian Institutes of Health Research fellow and doctoral student at Wilfrid Laurier University in Waterloo, Ontario, Canada exploring the gendered experiences of traumatic brain injury and the barriers and facilitating factors influencing mental health, well-being, and utilization of healthcare services encountered by women survivors of violence. She is also a practicing social worker, developing and implementing innovative individual and group-based interventions for people living with brain injury and chronic pain. As someone with lived experience of TBI, Lin has been engaged as a guest lecturer and panelist addressing issues of disability, brain injury, and marginalization for academic and community-based organizations internationally.
PANELIST: Halina (Lin) Haag, MSW, RSW is a Canadian Institutes of Health Research fellow and doctoral student at Wilfrid Laurier University in Waterloo, Ontario, Canada exploring the gendered experiences of traumatic brain injury and the barriers and facilitating factors influencing mental health, well-being, and utilization of healthcare services encountered by women survivors of violence. She is also a practicing social worker, developing and implementing innovative individual and group-based interventions for people living with brain injury and chronic pain. As someone with lived experience of TBI, Lin has been engaged as a guest lecturer and panelist addressing issues of disability, brain injury, and marginalization for academic and community-based organizations internationally.
 PANELIST: Heather Shepherd, BSc graduated from Queen’s University, Ontario, Canada, in June 2014. She majored in psychology and neuroscience and completed her final year of study at the University of St. Andrews in Scotland on a full academic scholarship. Heather has sustained numerous concussions both in sport and in everyday activities which have affected all aspects of her life.
PANELIST: Heather Shepherd, BSc graduated from Queen’s University, Ontario, Canada, in June 2014. She majored in psychology and neuroscience and completed her final year of study at the University of St. Andrews in Scotland on a full academic scholarship. Heather has sustained numerous concussions both in sport and in everyday activities which have affected all aspects of her life.
Oral Presentation of Scientific Papers — Pain Topics
THU // 2:00 PM – 3:30 PM
Moderator: Virgil Wittmer, PhD
2:00 -2:20: The Influence of Contextual Factors on Community Reintegration Among Injured Service Members (#1775)
Presented by Brent Hawkins
2:20 – 2:40: Behavioural Therapy combined with Physical Training improves function and diminishes pain in Chronic Back Pain (#1091)
Presented by Jan-Paul Wingerden
2:40 – 3:00: The Efficacy of Stabilization Exercise Combined With Transforaminal Epidural Steroid Injection for Lumbar Radiating Pain (#1933)
Presented by Ju Seok Ryu
Regenerative Medicine of Musculoskeletal Tissue: Bone, Cartilage, Disc, and Muscle #1310
THU // 2:00 PM – 3:30 PM
Faculty
Carmen militza Terzic, MD, PhD, Mayo Clinic, Rochester, MO; Nathan K. LeBrasseur, PhD, Mayo Clinic, Rochester, MO; Christopher H. Evans, PhD, Mayo Clinic, Rochester, MO; Wenchun Qu, MD, PhD, Mayo Clinic, Rochester, MO
Diagnosis/Area of Practice: Cross-Cutting/Frailty, spine disc disease, cartilage and bone degeneration
Focus: Outcomes research/epidemiology
Regenerative Medicine will be a vital component of medical and surgical practice in the coming years as it will create new models of health care and transform medicine and surgery. Therefore, it is important to educate the next generation of clinicians and scientists in the latest regenerative medicine applications. This symposium will provide an update on promising regenerative therapies and stem cell technology aiming to repair, regenerate, recover and restore skeletal muscle, bone, cartilage, and intervertebral disc.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Recognize novel therapies to restore skeletal muscle mass in the face of aging and disease
- Identify novel therapies to promote repair and regeneration of bone and cartilage
- Discuss the use of stem cell technologies for regenerative medicine in intervertebral disc disease
Electrical Stimulation Training in Persons With Spinal Cord Injury: Outcomes of Clinical Trials #1092
THU // 2:00 PM – 3:30 PM
Faculty
Ashraf S. Gorgey, PT, PhD, Hunter Holmes McGuire VA Medical Center, Richmond, VA; Gail F. Forrest, PhD, Rutgers New Jersey Medical School, Rutgers, the State University of New Jersey, Newark, NJ; Therese E. Johnston, PT, PhD, MBA, Jefferson School of Health Professions, Thomas Jefferson University, Philadelphia, PA
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The current symposium will discuss the health-related outcomes of recent clinical trials that utilized FES or NMES for both the upper and lower extremity in conjunction with resistance training, blood flow restriction, cycling, standing and walking on treadmill, and supine exercises in adults and children with SCI. The presented findings will allow rehabilitation specialists to modify and stream line their interventions to focus on rehabilitation strategies aimed at ameliorating muscle and bone loss after SCI. The outcomes of the training studies presented will develop a consensus on utilizing electrical stimulation for both upper and lower extremity rehabilitation after SCI.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss current NMES and FES multi-intervention applications to address skeletal muscle and bone adaptations, and the evidence for their use
- Understand the effects of NMES or FES multi-intervention applications on metabolic outcomes (basal metabolic rate, energy expenditure)
- Compare and contrast potential indications and outcomes from different FES and NMES trials
Rehabilitation Robotics and Neuro-Stimulation #1225
THU // 2:00 PM – 3:30 PM
Faculty
Hermano Igo Krebs, PhD, Massachusetts Institute of Technology, Cambridge, MA; Dylan Edwards, PhD, Weill Medical College of Cornell University, White Plains NY; Hermano Igo Krebs, Massachusetts Institute of Technology, Cambridge, MA
Diagnosis/Area of Practice: Stroke
Focus: Neuroscience (e.g., neural regeneration/repair, motor control/learning, biomechanics)
The field of rehabilitation robotics has grown steadily over the past decade, with significant clinical contributions. Studies have demonstrated both the efficacy and efficiency of robotics for assessing and treating motor impairment and function post-stroke although many questions remain. Likewise, the field of neuro-stimulation has grown steadily over the past decade although many questions remain. The purpose of this symposium is to provide a concise, yet broad-based introduction to key topics in rehabilitation robotics and neuro-stimulation, discuss evidence supporting the modalities, as well as attempts to augment rehabilitation outcomes and combine both approaches.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify need and basic concepts behind Rehabilitation Robotics and Neuro-Stimulation
- Discuss American Heart Association and VA Guidelines Post-Stroke on the use of therapeutic robots
- Discuss a few clinical results to support the AHA conclusions on the use of therapeutic robotics for stroke rehabilitation
- Discuss of Meta-Analyses and Evidence Supporting the Use of Neuro-Stimulation Post-Stroke
- Discuss the evidence on the potential of combining robotics and neuro-stimulation to enhance outcomes
Falls in Individuals with Multiple Sclerosis: Predictors, Consequences, and Prevention #1093
THU // 2:00 PM – 3:30 PM
Faculty
Jacob Sosnoff, PhD, University of Illinois at Urbana-Champaign, Urbana, IL; Michelle Cameron, MD, PT, Portland VA Medical Center, Oregon Health & Science University, Portland, OR; Elizabeth Peterson, PhD, OTR/L, University of Illinois at Chicago, Chicago, IL; Marcia Finlayson, PhD, OT Reg (Ont), OTR, Queen’s University, Kingston, ON, Canada
Diagnosis/Area of Practice: Neurodegenerative disease (e.g., MS, Parkinson’s disease)
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Multiple sclerosis (MS) is a chronic, often disabling neurodegenerative disease that is common among adults worldwide. This disease process involves intermittent bursts of focal inflammation across the central nervous system which results in damage throughout the nervous system. This nervous system damage is associated with a heterogeneous array of functional impairments and symptoms. Falls are common in persons with MS; approximately 60% of individuals with MS report falling in the previous 6 months. Understanding the risk factors, consequences and prevention of falls is an important step toward improving the rehabilitation process and outcomes for individuals with MS.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the factors associated with past and future falls in individuals with MS
- Discuss the consequences of falls in individuals with MS
- Discuss rehabilitative strategies to prevent falls in individuals with MS
- Identify next steps in MS fall research
Recognizing Imbalance and Fall Risk in Cancer Survivors #1150
THU // 2:00 PM – 3:30 PM
Faculty
Elizabeth Hile, PhD, PT, NCS, University of Pittsburgh School of Health and Rehabilitation Sciences, Pittsburgh, PA; Grace Campbell, PhD, MSW, CRRN, University of Pittsburgh School of Nursing, Allison Park, PA; Brian McMichael, MD, University of Pittsburgh School of Medicine, Pittsburgh, PA
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Emerging evidence suggests that cancer survivors are at increased risk for balance deficits, falls, and fractures. These impairments can interfere with return to pre-cancer social participation, prevent independence, lead to morbidity, and may even impact recurrence. Many survivors and healthcare providers are unaware of neurorehabilitative options to improve balance and manage fall risk. This symposium will review the evidence for cancer-related imbalance and falls risk, suggest a prospective surveillance model for monitoring mobility during cancer treatment, and discuss potential rehabilitative options to remediate such deficits. The speakers will also discuss knowledge gaps, opportunities for future research, and clinical implications.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the incidence of imbalance, falls, and subsequent injury in cancer survivors, and potential consequences impacting quality of life (disability, falls, restricted activity).
- Summarize main points from the existing published evidence in balance assessment, balance rehabilitation, fall detection, and fall prevention, with specific attention to the implications for advancing oncology rehabilitation.
- Describe a prospective surveillance model for balance impairment in individuals with cancer, and the potential for early rehabilitation to improve survivorship outcomes.
- Discuss the clinical implications of current published evidence and related pilot data presented by the speakers, recognizing opportunities to address knowledge gaps in an effort to advance oncology rehabilitation and subsequently long-term outcomes for cancer survivors.
Too Young for Therapy? Activity-Based Rehabilitation for Infants and Toddlers With Spinal Cord Injuries #1213
THU // 2:00 PM – 3:30 PM
Faculty
Janet Dean, MS, RN, CRRN, CRNP, International Center for Spinal Cord Injury, Kennedy Krieger Institute, Baltimore, MD; Kaitlin MacDonald, MOT, OTR/L, International Center for Spinal Cord Injury, Kennedy Krieger Institute, Baltimore, MD; Sarah Murdoch, PT, DPT, International Center for Spinal Cord Injury, Kennedy Krieger Institute, Baltimore, MD
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Pediatric Rehabilitation
Spinal cord injury (SCI) in infants and toddlers (0-3 years) is a rare occurrence that has lifelong consequences for child development and family life. This situation challenges rehabilitation professionals to create an environment to facilitate the acquisition of neurodevelopmental milestones in a setting of severe motor and sensory impairment. Case studies will be presented in order to illustrate the application of ABR with infants and toddlers with spinal cord injury. The use of advanced technology and therapeutic modalities, including the use of functional electrical stimulation as well as early independent mobility facilitates development and promotes neurological recovery.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Apply current literature regarding the importance of early activity and mobility in the acquisition of neurodevelopmental milestones in infants and toddlers with spinal cord injury
- Define the concept plasticity as it relates to the interaction of spinal cord injury and growth and development of infants and toddlers
- Define and apply Activity Based Rehabilitation principles using functional electrical stimulation and advanced technology for infants and toddlers
- Identify the importance of a lifelong, activity based home and community rehabilitation program for children with SCI, to minimize complications, facilitated development and promote neurological recovery
There is No Place Like Home: Identifying Strategies to Decrease Readmissions #1082
THU // 2:00 PM – 3:30 PM
Faculty
Pamela Roberts, PhD, OTR/L, SCFES, FAOTA, CPHQ, Cedars-Sinai Medical Center, Los Angeles, CA; Richard Riggs, MD, Cedars-Sinai Medical Center, Los Angeles, CA; Margaret A. DiVita, PhD, MS, Uniform Data Systems for Medical Rehabilitation, Amherst, NY
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Early identification of patients with conditions that place them at high risk for a readmission, combined with actionable risk-reduction strategies, has potential for a positive rehabilitation health care impact. This symposium will review current literature regarding readmissions, highlight best practices to reduce readmissions, as well as offer practical strategies to keep patients from returning to the hospital for avoidable readmissions.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Become familiar with current readmission evidence for both the acute hospital and post-acute care
- Increase awareness of how current research can effectively guide clinical practice in identifying readmissions medical and functional risk factors
- Describe strategies for prevention and reduction of medical and functional risk factors
Answering Global Challenges in International Health Care Systems: What Can We Learn From Each Other? #1158
THU // 2:00 PM – 3:30 PM
Faculty
Christine MacDonell, CARF International, Washington, DC; Christina May Moran de Brito, MD, PhD, Rehabiliutation Service of the Hospital Sirio-Libanes, Sao Paulo, Brazil; Lisandro E. Olmos, MD, FLENI Rehabilitation, Buenos Aires, Argentina; Hubert Vaugnat, MD, Geneva University Hospitals, Geneva, Switzerland; Raisa B. Deber, PhD, University of Toronto, Institute of Health Policy, Management, and Evaluation, Toronto, ON, Canada; Gerben DeJong, PhD, FACRM, Medstar National Rehabilitation Hospital, Washington, DC
Diagnosis/Area of Practice: Cross-Cutting
Focus: Health/disability policy, ethics, advocacy
This session will focus on four countries’ identification of challenges within the rehabilitation continuum, common approaches to rehabilitation, and chronic care and long-term care that may work across health systems. It will also address research actions to assist in answering the questions about effective and efficient care across culturally diverse health systems. Rehabilitation needs this dialogue and opportunities to improve the recognition of our value and assist in developing appropriate care models for the future.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify 3 features that differentiate various health systems and how they shape their responses to challenges
- Identify 2 cross country comparisons that could enhance policy changes going forward
- Identify 2 research questions that would facilitate cross cultural comparisons and improve the field of long term rehabilitation needs
Developing Best Practice in Rehabilitation for Patients With Severe Obesity #1130
THU // 2:00 PM – 3:30 PM
Faculty
Mary Forhan, University of Alberta, Edmonton, AB, Canada; Arya Sharma, University of Alberta, Edmonton, AB, Canada; Dawn Hatanaka, Canadian Obesity Network, Edmonton, AB, Canada
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The proportion of rehabilitation patients who have severe obesity is increasing. Health care professionals have identified gaps in knowledge about obesity and limited competency and capacity to provide safe, efficient and effective care for such patients. This symposium will provide an overview of the evidence for best practice in rehabilitation for patients with obesity and will share the results of an inter-professional bariatric care training program that has been effective in promoting the uptake of evidence about obesity and changing clinical practice in acute care, home care, and community care.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify factors that contribute to quality care for rehabilitation patients with severe obesity
- Reflect on their own practice to identify ways in which they contribute to quality care for their patients with severe obesity
- Identify gaps in knowledge about best practice in rehabilitation for patients with severe obesity
- Identify areas for further research needed to promote best practice for rehabilitation patients with severe obesity
Current Challenges With Spasticity Treatment: Road Blocks or Opportunities? #1154
THU // 2:00 PM – 3:30 PM
Faculty
Chetan P. Phadke, PT, PhD, West Park Healthcare Centre, University of Toronto, Toronto, ON, Canada; Pavel Lindberg, PT, PhD, INSERM French National Medical Research and Health Institute, Paris, France; Farooq Ismail, MD, West Park Healthcare Centre, University of Toronto, Toronto, ON, Canada; Chris Boulias, MD, PhD, West Park Healthcare Centre, University of Toronto, Toronto, ON, Canada; Karen Ethans, MD, Spinal Cord Injury Unit, University of Manitoba, Winnipeg, MB, Canada
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This Instructional Course will present findings associated with measurement of spasticity and function using clinical and research experience, including: (1) new technology that can offer a way for objective and reliable assessment of spasticity in the clinical setting, (2) clinical challenges and difficult cases associated with pharmacological interventions that will provide insights to both new and experienced clinicians, (3) research findings that help understand the environmental impact on spasticity, and (4) the impact of botulinum toxin injections on the muscle spindles (mechanism underlying spasticity) and provide future directions for research aimed at advancing spasticity management.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe challenges associated with spasticity management
- Discuss new approaches to measure spasticity
- Describe the impact of pharmacological interventions on mechanisms of spasticity
- Discuss the environmental impact on the experience of spasticity
Oral Presentation of Scientific Papers — Pain Topics
THU // 2:00 PM – 3:00 PM
Moderator: Virgil Wittmer, PhD
2:00 – 2:20: The Influence of Contextual Factors on Community Reintegration Among Injured Service Members (#1775)
Presented by Brent Hawkins
2:20 – 2:40: Behavioural Therapy combined with Physical Training improves function and diminishes pain in Chronic Back Pain (#1091)
Presented by Jan-Paul Wingerden
2:40 – 3:00: The Efficacy of Stabilization Exercise Combined With Transforaminal Epidural Steroid Injection for Lumbar Radiating Pain (#1933)
Presented by Ju Seok Ryu
NETWORKING BREAK // EXPO
THU // 3:30 PM – 4:00 PM
BI-ISIG: Cognitive Rehabilitation Task Force Meeting
THU // 4:00 PM – 5:30 PM
Minimal Competency Guidelines for Rehabilitation of Persons With Disorders of Consciousness #1103
THU // 4:00 PM – 5:30 PM
Faculty
Risa Nakase-Richardson, PhD, Polytrauma Rehabilitation Program at James A. Haley VAMC, Tampa, FL; John Whyte, MD, PhD, Moss Rehabilitation Research Institute, Elkins Park, PA; Joseph T. Giacino, PhD, Spaulding Rehabilitation Hospital, Boston, MA; Douglas I. Katz, MD, Boston University School of Medicine, Boston, MA; Brian D. Greenwald, MD, Center for Head Injuries, JFK Johnson Rehabilitation Institute, Edison, NJ; Nathan D. Zasler, MD, FAAPM&R, FAADEP, DAAPM, CBIST, Concussion Care Centre of Virginia, Ltd, Richmond, VA; Theresa Louise-Bender Pape, DrPH, MA, CCC-SLP/L, Edward Hines Jr. Veterans Administration (VA) Research Service, Hines, IL; Amy Shapiro-Rosenbaum, PhD, Park Terrace Care Center, Queens, NY
Diagnosis/Area of Practice: Brain Injury
Focus: Health/disability policy, ethics, advocacy
Growing evidence supports the need for defining rehabilitation treatment and benefit for DOC survivors. DOC experts representing the ACRM, VA, and NIDRR TBI Model Systems have developed minimal competency guidelines for the rehabilitation of persons with DOC that address emerging areas of need in the scientific literature that ultimately impact patient care. The purpose of this symposium is to review the state of rehabilitation for persons with DOC and present key content areas of the minimal competency guidelines for their rehabilitation. A panel discussion will follow for audience comments and questions.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the current state of the science for rehabilitation potential of persons with DOC
- List at least three content domains for the minimal competency guidelines for persons with DOC
- Discuss rationale behind at least three key content domains of the minimal competency guidelines
- List common ethical issues facing persons with DOC during acute and chronic stages addressed in the minimal competency guidelines
Aging and Long-Term Issues Following Traumatic Brain Injury #1102
THU // 4:00 PM – 5:30 PM
Faculty
Mel B. Glenn, MD, Spaulding Rehabilitation Hospital, Harvard Medical School, Boston, MA; Kristen Dams-O’Connor, PhD, Brain Injury Research Center, Mount Sinai School of Medicine, New York, NY
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Studies on the medical, physical, cognitive, psychological, and social outcomes suggest increased vulnerability as people age following TBI. Studies are mixed with respect to the risk for dementia. There is evidence that multiple concussions predispose to cognitive decline. New information is emerging on the relationship of the pathological findings of chronic traumatic encephalopathy to emotional, behavioral, and cognitive disorders. Life expectancy is decreased in people with TBI, and there are dramatic increases in risk for certain causes of death in particular. However, there are medical, rehabilitation, and lifestyle interventions that can address many of these areas of vulnerability.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Summarize long-term areas of vulnerability for people with traumatic brain injury
- Identify the pathological entities associated with cognitive and behavioral changes following multiple concussions and subconcussions
- Compare the risk associated with various causes of death in people with traumatic brain injury with those seen in the general population
- Identify opportunities for intervention to improve function or prevent decline as people age with traumatic brain injury
Depression After SCI: State of the Science for Researchers and Practical Information for Clinicians #1274
THU // 4:00 PM – 5:30 PM
Faculty
Charles Bombardier, PhD, University of Washington School of Medicine, Seattle, WA
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Major depression (MDD) is a common, disabling secondary condition in people with spinal cord injury (SCI) that is undertreated. Recent research provides some guidance regarding: (1) how to efficiently screen for MDD in people with SCI, (2) what treatment approaches are preferred and effective, (3) how to monitor response to interventions and use the information to guide treatment decisions, and (4) how we might improve overall depression treatment effectiveness in real-world settings.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the psychometric properties of a depression screening measure that is valid in people with SCI
- Describe a means of measuring depression treatment improvement, response, and remission in SCI
- Describe preferred and promising depression treatment approaches for people with SCI
- List key elements of collaborative care, an approach to improve depression treatment effectiveness
Hot Topics in Stroke Rehabilitation: Differences in Models of Stroke Rehabilitation Across International Settings #2260
THU // 4:00 PM – 5:30 PM
Moderator: Christine MacDonell, Medical Rehabilitation and International Aging Services/Medical Rehabilitation, CARF International, Washington, DC
Participants
Ahmed AboAbat, PhD, BScPT, MHA, Rehabilitation Hospital, King Fahad Medical City, Saudi Arabia; Sharon Hartl, BS, OTR/L, Therapy Operations, New England Rehabilitation Hospital of Portland, Portland, ME; Judy Murray, MScPT, District Stroke Centre, Mackenzie Health, Richmond Hill, ON, Canada; Prathap Raghavan, MD, FRCPC, Physical Medicine and Rehabilitation, Royal Inland Hospital, Kamloops, BC, Canada
Diagnosis/Area of Practice: Stroke
Focus: Clinical Practice
The Stroke Interdisciplinary Special Interest Group and the International Networking Group are pleased to sponsor the 2014 Hot Topics in Stroke Rehabilitation Symposium. Come and participate in a lively discussion on similarities and differences in stroke rehabilitation across international settings. The moderated panel will present an overview on the timing, content, duration and funding of rehabilitation after stroke, as well as drivers of models of rehabilitation practice, from the perspective of three international systems of care (Canada, Saudi Arabia, United States). We will discuss unique features of each and identify those that show promise for broader application to elevate the quality and consistency of stroke rehabilitation world-wide. This symposium will offer unique opportunities to identify and stimulate international collaborations in practice, training, and research.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe models of stroke rehabilitation in three international settings
- Compare and contrast practices across the continuum of care
- Discuss opportunities for international exchange that may inform best practices in stroke rehabilitation
Cognitive and Brain Control of Mobility in Normal and Pathological Aging #1186
THU // 4:00 PM – 5:30 PM
Faculty
Joe Verghese, MMBS, MS, Albert Einstein College of Medicine, Bronx, NY; Gilles Allali, MD, visiting scientist at the Albert Einstein College of Medicine, Bronx, NY; Jeannette Mahoney, PhD, Albert Einstein College of Medicine, Bronx, NY; Roee Holtzer, PhD, Albert Einstein College of Medicine, Bronx, NY; Helena Blumen, PhD, Albert Einstein College of Medicine, Bronx, NY
Diagnosis/Area of Practice: Neurodegenerative disease (e.g., MS, Parkinson’s disease)
Focus: Other
Mobility impairments are common among older adults and are associated with increased risk of disability and mortality. Identifying cognitive and neural mechanisms of mobility can have major impact on risk assessments and interventions that are designed to optimize early detection and amelioration of mobility decline, respectively. Herein we provide a targeted survey of interdisciplinary research that is focused on the relationship between cognitive functions and mobility and their underlying neural substrates in normal and pathological aging.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the epidemiology of mobility impairments in normal and pathological aging
- Describe the relationship between cognitive status and functions with mobility in aging
- Discuss the neural substrates of mobility using traditional and novel neuroimaging methods
Multidisciplinary Pain Programs in Norway and Denmark with a Focus on Return to Work #2088
THU // 4:00 PM – 5:30 PM
Faculty
Toril Dale, Cand. Polit., AiR, National Center and Advisory Unit for Occupational Rehabilitation, Rauland, Norway; Irene Øyeflaten, National Centre for Occupational Rehabilitation, Norway; Chris Jensen, PhD, National Centre for Occupational Rehabilitation, Norway; Gro Karsten Skarholt, Rehabilitation Center AiR Clinic, Norway
Diagnosis/Area of Practice: Pain
Focus: Outcomes research/epidemiology
Norway and Denmark provide high public compensation benefits during sick leave and focus on interventions that may facilitate return to work. Multidisciplinary programs targeting return to work outcomes have been implemented in the health care sector for subacute and chronic pain patients. This symposium will address the Scandinavian context, and describe the interventions and outcomes. Uncertainty about target groups for interventions in the secondary health sector is a major challenge which will be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss National context differences
- Discuss universal return to work challenges
- Discuss the importance of pain in work rehabilitation
Evidence-Informed Intervention Approaches to Help Cancer Survivors Self-Manage Cognitive and Behavioral Concerns #1163
THU// 4:00 PM – 5:30 PM
Faculty
Mary Vining Radomski, PhD, OTR/L, Courage Kenny Research Center, Minneapolis, MN; Robert J. Ferguson, PhD, Eastern Maine Medical Center, University of Maine, Bangor, ME; Kathleen Lyons, ScD, OTR/L, Geisel School of Medicine, Dartmouth College, Lebanon, NH
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Some people experience cognitive and behavioral disturbances such as forgetfulness, fatigue, and anxiety that interfere with performance of self-management roles and activities during and/or after their cancer treatments. There is increasing evidence that rehabilitation interventions can contribute to cognitive and behavioral symptom management and support advance to normal living for these individuals. In this presentation, we will summarize the self-management problems associated with cognitive and behavioral issues experienced by some cancer survivors and describe contemporary explanatory theories. Researchers will also describe their approaches to and outcomes for 3 rehabilitation interventions that are either currently or recently under study.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss cognitive-behavioral disturbances experienced by some cancer survivors
- Summarize explanatory models for these problems and evidence associated with rehabilitation interventions
- Describe 3 intervention approaches that are currently or recently under study
Brain Injury Before Age Five: Implications for Rehabilitation #1155
THU // 4:00 PM – 5:30 PM
Faculty
Angela Hein Ciccia, PhD, CCC-SLP, Case Western Reserve University, Cleveland, OH; Julie Haarbauer-Krupa, PhD, Children’s Healthcare of Atlanta, Emory University School of Medicine, Atlanta, GA; Stacy Suskauer, MD, Kennedy Krieger Institute, Johns Hopkins University School of Medicine, Baltimore, MD
Diagnosis/Area of Practice: Brain Injury
Focus: Pediatric Rehabilitation
Identification, assessment, and management of the very young child (0-5 years of age) after brain injury is complicated and the process of rehabilitation is confounded by a multitude of variables that are unique to this age group. The aim of this symposium is discuss a subset of these factors with a focus on identifying barriers to access to care for young children with brain injury and to characterize how behavioral presentation after TBI may require broader consideration. The panel will then lead a discussion focused on suggestions for improving clinical practice and needed areas of research for this group.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify barriers to access to care for very young children with brain injury
- Identify aspects of unusual presentation/symptomatology for very young children with brain injury that contribute to under-identification
- Identify areas of research/improvements in clinical practice that would improve rehabilitation for very young children with brain injury
Developing and Reporting Research Evidence That Makes a Difference in Systematic Reviews #1273
THU // 4:00 PM – 5:30 PM
Faculty
Ronald T. Seel, PhD, FACRM, Crawford Research Institute, Shepherd Center, Atlanta, GA; Allen W. Heinemann, PhD, ABPP (RP), FACRM, Feinberg School of Medicine, Northwestern University, Chicago, IL; Leighton Chan, MD, MPH, National Institutes of Health, Bethesda, MD; Jacob Kean, PhD, Roudebush VA Medical Center/Regenstrief Institute, Indiana University School of Medicine, Indianapolis, IN
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Many rehabilitation studies and systematic reviews have significant methodological or statistical shortcomings, either in their reporting or design, which increase the risk of biased findings and prevent findings from being used in rehabilitation reviews and practice guidelines. This symposium, co-sponsored by the ACRM Evidence and Practice Committee and Outcome Measurement Networking Group, will provide evidence on the most common shortcomings in the reporting or design of each study type and review key criteria from the CONSORT, STARD, STROBE, and PRISMA reporting guidelines that will increase the likelihood that study findings will make a difference in systematic reviews and practice guidelines.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify common shortcomings in the design and/or reporting of clinical trials, diagnostic validity studies, observational and prognostic studies, and systematic reviews.
- Describe key reporting criteria in the CONSORT, STARD, STROBE, and PRISMA reporting guidelines and checklists.
- Evaluate the evidence for using mandated reporting criteria and associated clinical trial, diagnostic validity study, and prognostic validity study design strategies, and systematic review and practice guideline development strategies.
- Find resources, websites, and published references for reporting guidelines and evidence grading systems to improve the development, reporting, and evaluation of research evidence
Advances in Psychosocial Rehabilitation: Social Integration and Community Participation in Vulnerable Populations #1234
THU // 4:00 PM – 5:30 PM
Faculty
Alexander Libin, PhD, District of Columbia Veterans Affairs Medical Center, Chevy Chase, MD; Shirley Groer, PhD, US Veteran Affairs, Washington, DC, Washington, DC; Joel Scholten, MD, Washington DC VA Medical Center, Washington, DC; Manon Schalden, PhD, District of Columbia Veterans Affairs Medical Center, Baltimore, MD; Ellen K. Danford, DC VAMC, Washington, DC
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The symposium focuses on a Social Integration and Community Participation framework for best practices in medical rehabilitation, specifically chronic health conditions, neurorehabilitation, and impairments in civilians and OEF/OIF/OND veterans. Psychosocial research supported by the US Department of Veterans Affairs fosters a discussion about the cross-cutting, evidence-based topics in specialty areas as the basis for an integrated model of practice and educational programs for health care providers. The inter-organizational Well-Being Literacy, Multimedia Education and Psychosocial Research Program (WeLL) VAMC offers examples of rehabilitation and community integration care with the services available to vulnerable individuals with traumatic brain injury, spinal cord injury, and associated mental conditions.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify a Social Integration and Community Participation framework for best practices in medical rehabilitation, more specifically, chronic health conditions, neurorehabilitation, and impairments due to the impact of war (e.g. in OIF/IEF/OND returning veterans)
- Foster a discussion about the cross-cutting, evidence-based topics in specialty areas, e.g. acute, post-acute, and home/community-based services, as the basis for an integrated model of practice and educational programs for health care providers
- Exchange information relevant to Social Integration and Community Participation in Vulnerable Clinical Populations and synthesize these findings and observations
Development, Implementation and Sustainability of an Early Mobilization Program for Critically Ill Adult Oncology Patients #1206
THU // 4:00 PM – 5:30 PM
Faculty
Shari Frankel, MBA, PT, ATC, MD Anderson Cancer Center, Houston, TX; Mary Lou Warren, DNP, RN, CNS-CC, MD Anderson Cancer Center, Houston, TX
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Early mobilization in critically ill patients has emerged as an effective and evidence-based prevention strategy for several of the complications associated with immobility. The presentation will describe a detailed multidisciplinary program that was created at MD Anderson Cancer Center for the development, implementation, and sustainability of an early mobilization program with critically ill oncology patients in a mixed medical and surgical 54 bed ICU. A change of culture occurred in the Oncologic Intensive Care Unit with increased mobilizations performed by nursing and therapist. Case studies will be presented in the rehabilitation of critically ill cancer patients.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify effects of immobility on patients in intensive care units
- Discuss the benefits of early mobility to patients in intensive care units
- Identify barriers for implementing an early mobilization program
- Describe components of an adult ICU early mobilization program
- Discuss outcomes and sustainability of a model program
Social Media: The Emerging Source for Expert Advice for Persons With Disabilities #1279
THU // 4:00 PM – 5:30 PM
Faculty
Julie Gassaway, MS, RN, Shepherd Center, Atlanta, GA; Xinsheng Cai, PhD, American Institutes for Research, Washington, DC; Minna Hong, Shepherd Center, Atlanta, GA; John Morris, PhD, Shepherd Center, Atlanta, GA; Claire Cahow, CTRS, Craig Hospital, Englewood, CO
Diagnosis/Area of Practice: Cross-Cutting
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
Social media provides a mechanism for conversations with end-users (peers) who have “been there, done that” and become “experts” on how to overcome the challenges of living with a disability. Its use can increase self-efficacy and appropriate resource utilization when participants can learn and brainstorm ideas with the peers. It also establishes social networks that increase community participation. Social media has found its way into the rehabilitation process and life-long communication venues for persons with disabilities. Rehabilitation centers can benefit from capitalizing on the power of social media.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand how social media can help to infuse appropriate information related to medical issues into commonly used non-medical sources
- Develop ideas of how to disseminate research results through social media channels
- Understand use of social media during emergencies by people with disabilities
- Observe well-constructed video presentation examples of social media used within disabled communities
Oral Presentation of Scientific Papers — Outcomes Measurement/Brain Injury Topics
THU // 4:00 PM – 5:30 PM
Moderator: Claire Kalpakjian, PhD
4:00 – 4:20: Impact of Anxiety on Post-Hospital Traumatic Brain Injury Rehabilitation Outcomes: A Prospective cohort study (#1625)
Presented by Gordon Horn
4:20 – 4:40: Dimensions that Characterize Recovery from Traumatic Brain Injury During the Post-acute Period (#1810)
Presented by Mark Sherer
4:40 – 5:00: Systematic review of prognostic models for mild traumatic brain injury (#1822)
Presented by Noah Silverberg
5:00 – 5:20: Cortical Thickness Changes of Individuals With Chronic Traumatic Brain Injury Following Strategy-Based Reasoning Training (#2033)
Presented by Kihwan Han
 |
 |
|
 |
EXHIBITORS WELCOME RECEPTION & POSTER VIEWING
THU // 5:30 PM – 7:00 PM
FREE Ticketed Event
Expand your learning experience at the Exhibitors Welcome Reception and Poster Viewing. Come to the Expo and discover the latest technologies, equipment, products and publications, services, and business solutions to meet your needs, and register to WIN exciting prizes and giveaways.
Engage with poster authors in a casual setting and learn about their latest research findings as you visit the Poster Display area. Don’t miss this exciting evening of discovery!
FRIDAY, 10 OCTOBER 2014
Expo Open // 10:00 AM – 2:00 PM
ACRM SPECIAL INTEREST & NETWORKING GROUP MEETINGS
Stroke-ISIG: Movement & Interventions Task Force Meeting
FRI // 7:00 AM – 8:00 AM
BI-ISIG: Disorders of Consciousness Task Force General Meeting
FRI // 7:00 AM – 8:00 AM
BI-ISIG: Pediatric & Adolescent Task Force Meeting
FRI // 7:00 AM – 8:00 AM
Early Career Networking Group Business Meeting
FRI // 7:00 AM – 8:30 AM
[sm_hr]
SPONSORED BREAKFAST [label style=”important”]CANCELLED[/label]
FRI // 7:15 AM – 8:15 AM
FREE Ticketed Event
Identifying the Active Ingredients and Outcomes of Discipline-Specific Therapy in Traumatic Brain Injury Rehabilitation #1247
FRI // 8:30 AM – 10:00 AM
Faculty
Clare Giuffrida, PhD, OTR/L, FAOTA, Rush University Medical Center, Chicago, IL; Janet M. Powell PhD, OTR/L, FAOTA, University of Washington, Seattle, WA; James Young, MD, Rush University Medical Center, Chicago, IL; Cynthia L. Beaulieu, PhD, ABPP-CN, Brooks Rehabilitation Hospital, Jacksonville, FL: Susan D. Horn, PhD, Institute for Clinical Outcomes Research, Salt Lake City, UT; Misti Timpson, DPT, NCS, CBIS, Rocky Mountain University of Health Professions, Provo, UT; Teri Sommerfeld, RN, CRRN, MHA, FACHE, Rush University Medical Center, Chicago, IL; Christopher Reddin, PhD, RN, CEN, United States Navy, San Diego, CA
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Understanding what patients do daily in rehabilitation therapies is essential for identifying which activities or combinations of activities are associated with best outcomes. This symposium describes an innovative research methodology, Practice Based Evidence, as used in the Traumatic Brain Injury (TBI) – Practice Based Evidence Project (PBE). By using Point of Care documentation, this project uniquely captures active ingredients of inpatient TBI rehabilitation across rehabilitation disciplines and length of stay. Signature practice patterns for each discipline, as well as specific occupational therapy activity intervention combinations, and their relationship to functional outcomes for different cognitive TBI groups are examined.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe how practice-based evidence methodology is useful in capturing and identifying critical elements of acute TBI rehabilitation
- Compare the PBE research findings relating to therapy activities following stroke and spinal cord injury to TBI-PBE findings
- Describe the development and implementation of Comprehensive Severity Index (CSI) and Point of Care (POC) documentation across the rehabilitation disciplines in the TBI PBE study to capture the critical elements of day to day therapeutic intervention for persons with TBI
- List the discipline-specific therapy activities that are most frequently engaged in within cognitively homogenous patient groupings across the acute rehabilitation stay for TBI
- Discuss the relationship of the salient occupational therapy activity-intervention combinations as captured through the Point of Care documentation to functional outcomes in persons with TBI by age and cognitive grouping
Concussion and Students: An Inter-Professional Approach to Concussion Management #1214
FRI // 8:30 AM – 10:00 AM
Faculty
Michael G. Hutchison, PhD, David L. MacIntosh, Sport Medicine Clinic, University of Toronto, Toronto, ON, Canada; Barbara Csenge, BEd, Learning Enrichment Centre, St. Michael’s College School, Toronto, ON, Canada; Paul Comper, Phd, CPsych, Toronto Rehab, University Health Network, Toronto, ON, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The majority of concussions occur to school aged children where return-to-school and learning environments should be the priority. This symposium will provide an overview of an innovative inter-professional approach to support students returning to school activity after concussion. This unique program of a sports medicine concussion clinic, research institution, and an independent boys school, has supported over 300 student concussions. The symposium will review medical principles when managing students with concussions, specifically drawing on our institution’s Rules to Recovery. We will also provide an in-depth examination from the school’s perspective of what should be included in a comprehensive concussion strategy.
Emerging Biological Targets for Spinal Cord Repair and Regenerative Rehabilitation #1170
FRI // 8:30 AM – 10:00 AM
Faculty
Isobel A. Scarisbrick, PhD, Rehabilitation Medicine Research Center, Mayo Clinic, Rochester, MN; Michael G. Fehlings, MD, FACs, FRCSC, PhD, University of Toronto, Toronto Western Hospital, University Health Network, Toronto, ON, Canada; Andrea J. Mothe, PhD, Toronto Western Hospital, University Health Network, Toronto, ON, Canada; Cindi M. Morshead, PhD, University of Toronto, Toronto, ON, Canada
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Neuroscience (e.g., neural regeneration/repair, motor control/learning, biomechanics)
SCI is a challenging clinical entity because the CNS has limited capacity for repair and regeneration. The pathophysiology of SCI is complex, but recent insights into pivotal cellular and molecular players have spawned a new era in which pharmacotherapies applied in the days and months after injury may prevent neural degeneration and promote neural- and neuroglial-regeneration. In addition, neural cell replacement strategies offer great promise alone or in combination with pharmacotherapy and rehabilitation. This symposium will provide an overview of cellular and molecular targets with potential for clinical translation to improve function in SCI patients.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify new neuroprotective and neuroregenerative targets for the treatment of spinal cord injury
- Understand new stem cell therapies being developed to regenerate the injured spinal cord
- Discuss new therapies in clinical trial to repair the injured spinal cord
Conceptual Framework for the Study of Sleep Disturbance Following Acute Neurologic Injury #1126
FRI // 8:30 AM – 10:00 AM
Faculty
Risa Nakase-Richardson, PhD, MHBS James A. Haley Veterans Hospital, University of South Florida, Tampa, FL; Ross Zafonte, DO, Harvard Medical School, Spaulding Rehabilitation Network, Boston, MA; Michael J. Makley, MD, Craig Hospital, Englewood, CO
Diagnosis/Area of Practice: Stroke/Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Persons with chronic brain injury demonstrate a greater prevalence of sleep disorders; however, little is known about the prevalence and impact on acute neurologic recovery. Animal and human studies have shown that sleep-wake cycle disturbances may alter neural function as well as physical functioning, mood, cognition and behavior. Sleep is critical for neural repair in early stages of recovery and disordered sleep may play a greater role in influencing outcome than previously understood. The purpose of this symposium is to present a series of talks by presenters from various disciplines promoting a conceptual framework for future study of acute sleep disturbances.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- List common sleep disorders observed during acute neurorehabilitation
- Describe outcomes associated with acute sleep disturbance
- List mechanisms of recovery influenced by disordered sleep
- Identify key elements of the therapeutic milieu required for promoting restorative sleep on the rehabilitation unit
Pediatric MS: Outcomes and Interventions #1222
FRI // 8:30 AM – 10:00 AM
Faculty
E. Ann Yeh, MD, University of Toronto, Toronto, ON, Canada; Brenda Banwell, MD, Children’s Hospital of Philadelphia, University of Pennsylvania, Philadelphia, PA; Lauren Krupp, MD, National Pediatric MS Center, SUNY, Stony Brook, NY; Christine Till, PhD, York University, Toronto, ON, Canada
Diagnosis/Area of Practice: Neurodegenerative disease (e.g., MS, Parkinson’s disease)
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Up to 2/3 of children with MS will experience accompanying depression and fatigue, while MRI and longitudinal neurocognitive studies suggest progressive decline within 3 years of onset. In this symposium, after providing an overview of pediatric MS and demyelinating disorders, we will discuss neurocognitive and psychosocial outcomes in these conditions. Specific attention will be paid to cutting edge scientific research on structural and functional MRI correlations with cognitive and psychosocial outcomes. Current evidence for pharmacologic and non-pharmacologic treatment of symptoms in this population will be discussed, including modalities such as exercise and cognitive rehabilitation.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify current diagnostic criteria for pediatric demyelinating disorders.
- Describe the clinical and MRI presentation of pediatric MS
- Describe the neurocognitive and psychosocial trajectory of children with MS
- Describe the relationship between structural changes in the brain and neurocognitive outcomes in this population
- Discuss evidence for non-pharmacologic and pharmacologic interventions for the symptomatic management of pediatric MS
Pain Catastrophizing and Fear Avoidance of Movement #1292
FRI // 8:30 AM – 10:00 AM
Faculty
Virgil T. Wittmer, PhD, Brooks Rehabilitation, Jacksonville, FL; Sara Bertoch, PhD, Rehabilitation Institute of Chicago, Center for Pain Management, Chicago, IL; Steven Stanos, DO, Center for Pain Management, Rehabilitation Institute of Chicago, Chicago, IL; Elizabeth Gaffron, MOTR/L, LMT, Rehabilitation Institute of Chicago, Chicago, IL
Diagnosis/Area of Practice: Pain
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Pain catastrophizing is a cognitive variable which has proven to be a significant predictor for development of a dysfunctional response to pain. Research has also found that the fear avoidance model of chronic pain, which includes pain catastrophizing, strongly correlates with physical disuse, depression, and disability over time. The medical model approach for treatment of subacute to chronic pain has been proven to be ineffective; therefore, there is a need to identify as well as treat irrational (catastrophic) thoughts as well as dysfunctional (fear-avoidance) behaviors in order to prevent development of a chronic pain syndrome. This requires an integrated rehabilitation and biopsychosocial perspective, rather than a “silo” approach to treatment.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the relationship between pain catastrophizing and fear-avoidance of movement
- Discuss research strongly suggesting that pain catastrophizing and fear (especially regarding increased pain) are significant predictors of disability and physical disuse
- Become familiar with questionnaires used to measure pain catastrophizing and fear-avoidance
- Discuss basic interdisciplinary rehabilitation treatment strategies for patients high in fear and pain catastrophizing
Treating People With Cancer: Opportunities for Professionals Exist, But What are the Learning Needs? #1208
FRI // 8:30 AM – 10:00 AM
Faculty
Oren Cheifetz, PhD, Canadian Cancer Rehabilitation and Education Institute, Hamilton, ON, Canada; Jan Park Dorsay, RN(EC), MN, CON(C), RMFT, Canadian Cancer Rehabilitation and Education Institute, Hamilton, ON, Canada; Amanda Smart, PT, MSc PT, Canadian Cancer Rehabilitation and Education Institute, Hamilton, ON, Canada
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
While evidence is showing the potential impact of exercise on reducing the risk of recurrence for several types of cancers, the burden of disease and costs to the health care system remain. The role of health care providers in cancer rehabilitation is evolving and the need for expertise in this area is likely to increase. Attendance at this session will assist professionals to identify potential learning needs with respect to working with people with cancer and the resources available to address those needs.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the recent evidence supporting the use of exercise with people diagnosed with cancer
- Provide a framework for self-reflection and assessment of knowledge and skills prior to working with people with cancer
- Demonstrate strategies and identify resources professionals can use to meet identified learning needs related to working with this growing, complex population
Methodological Issues in Mild Traumatic Brain Injury Research: A Workshop #1263
FRI // 8:30 AM – 10:00 AM
Faculty
Vicki Leigh Kristman, Lakehead University, Thunder Bay, ON, Canada; Connie Marras, University Health Network, University of Toronto, Toronto, ON, Canada; Cesar Hincapie, University Health Network, University of Toronto, Toronto, ON, Canada; James Donovan, University Health Network, University of Toronto, Toronto, ON, Canada; J. David Cassidy, University Health Network, University of Toronto, Toronto, ON, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
The methodological quality of the research literature on mild traumatic brain injury prognosis has been slow to develop. Improved identification and avoidance of methodological flaws in research studies are needed. This symposium will provide an overview of the common methodological concerns found in prognostic studies of mild traumatic brain injury, offer recommendations on how to avoid these common flaws, and give participants the opportunity to identify and discuss the methodological issues addressed through review of a published paper. Improving the quality of studies will aid understanding of mild traumatic brain injury prognosis and assist clinicians in educating and treating patients.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify common methodological issues in the MTBI prognostic literature
- Discuss the concepts behind the methodologic issues
- Suggest research study designs and methods for avoiding these issues
- Apply this knowledge to the development of research protocols addressing MTBI prognosis
Navigating US Post-Acute Care Policy: Where Do I Begin? #1195
FRI // 8:30 AM – 10:00 AM
Faculty
Holly DeMark Neumann, MPPA, CCRC, Rehabilitation Institute of Chicago, Chicago, IL; Anne Deutsch, PhD, RN, CRRN, Rehabilitation Institute of Chicago, Chicago, IL; Deborah Backus, PT, PhD, Eula C. and Andrew C. Carlos MS Rehabilitation and Wellness Program, Shepherd Center, Atlanta, GA; Dahlia Shaewitz, AIR and Model Systems Knowledge Translation Center, Washington, DC
Diagnosis/Area of Practice: Cross-Cutting
Focus: Health/disability policy, ethics, advocacy
Navigating the world of healthcare policy may seem overwhelming for busy clinicians and researchers. In this course, we introduce the key terminology and organizations involved in post-acute care policy development and implementation. We arm clinicians and researchers with strategies for keeping informed of key policy decisions, as well as engaging policymakers to discuss policy implications of research projects.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Define key terminology used in post-acute care policy-making
- Identify key organizations and stakeholders in post-acute care policymaking
- Describe strategies for clinicians and researchers to engage with policymakers
Integrating Assistive Technology into Rehabilitation Programming: Successes and Challenges #1153
FRI // 8:30 AM – 10:00 AM
Faculty
Risa Nakase-Richardson, PhD, Veterans Affairs, James A. Haley Veterans Hospital, Tampa, FL; Brian W. Schulz, PhD, Rehabilitation Engineering and Prosthetics/Orthotics Rehabilitation Research and Development Service, VA Office of Research and Development, Tampa, FL; Linda Resnik, PT, PhD, Providence VA Medical Center, Brown University, Providence, RI; Tessa Hart, PhD, Moss Rehabilitation Research Institute, Elkins Park, PA; Charles Levy, MD, VA Center of Innovation on Disability and Rehabilitation Research, North Florida/South Georgia Veterans Health System, Gainesville, FL
Discussant: Marcia J. Scherer, PhD, MPH, FACRM, Institute for Matching Person & Technology, Webster, NY
Diagnosis/Area of Practice: Cross-Cutting
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
Rehabilitation has expanded beyond provision of individualized in-person cognitive, motor, and behavioral therapies and the prescription of simple assistive devices. Today’s advances include prescription and training with a wide assortment of complex assistive technology. The process of individualizing prescription and training for persons with variable deficits requires an understanding of patient cognition, patient and provider access and acceptance of technology, and an appreciation of the evolving nature of the field. This symposium will highlight studies using AT in rehabilitation. Final comments regarding novel applications, appropriate prescription, and future directions of research will be provided by Dr. Marcia Scherer.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- List cognitive challenges with use of technologically complex devices
- Describe how everyday technology may be used for alleviating psychological distress after brain injury
- List patient characteristics associated with greater benefit from cognitive tele-rehabilitation
- Discuss at least 2 major considerations when matching persons with technology
- Describe the challenges and opportunities for use of telehealth to deliver rehabilitation to the home setting
Telerehabilitation: A New Frontier in Geriatric Rehabilitation # 1177
FRI // 8:30 AM – 10:00 AM
Faculty
Deirdre Dawson, PhD, OT Reg (Ont), Rotman Research Institute, Baycrest, University of Toronto, Toronto, ON, Canada; Helen Hoenig, MD, MPH, Durham VA Medical Center, Duke University Medical Center, Durham, NC; Nancy Latham, PhD, PT, Health and Disability Research Institute, Boston University School of Public Health, Boston, MA; Emily Nalder, PhD, OT, Rotman Research Institute, Baycrest, Toronto, ON, Canada
Diagnosis/Area of Practice: Cross-Cutting/Geriatric Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
E-health, or the delivery of online interventions, has the potential to improve access to quality health care services for older adults by providing timely services in their own home for a variety of interventions. Accumulating evidence suggests that e-health applications are beneficial for a variety of health conditions. This presentation will review the evidence for web-based interventions for older adults, present findings related to four applications of telehealth, and discuss the experiences of health care professionals transitioning from face to face to online interactions with clients. Case examples will be provided and clinical applications discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Become familiar with various platforms that can used for telerehabilitation interventions
- Gain knowledge regarding several unique telehealth clinical programs for use with older adults
- Consider facilitators and barriers to uptake of e-health programs by health professionals and their clients
- Discuss clinical implications of programs presented and key directions for future research
New Trends in the Care and Rehabilitation of Chronic and Complex Medical Conditions #1313
FRI // 8:30 AM – 10:00 AM
Faculty
Carmen militza Terzic, MD, PhD, Mayo Clinic, Rochester, MO; Kristin D. Zhao, PhD, Center for Rehabilitation Medicine Research, Mayo Clinic, Rochester, MO; Andrea L. Cheville, MD, Center for Rehabilitation Medicine Research at Mayo Clinic, Rochester, MO; Jeffrey R. Basford, MD, PhD, Mayo Clinic, Rochester, MO
Diagnosis/Area of Practice: Cross-Cutting/Chronic and complex diseases, musculoskeletal disorders
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Patients with complex and chronic conditions are more often a part of the Rehabilitation Medicine practice; therefore, it is imperative that we address chronic conditions that affect their quality of life and cost effective follow up and treatment of these patients are necessary. Here we review the use of novel functional patient-reported outcomes (PROs) to assist in decision making for patients with complex and chronic conditions. We will also discuss home-exercise intervention provided via tele-rehabilitation. The growing capability of new techniques such as magnetic resonance elastography to address chronic conditions such as fibromyalgia and myofascial pain syndrome will be reviewed as well.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Recognize the importance of functional patient-reported outcomes in the care of complex and chronic medical conditions
- Cite new generation of patient-reported outcomes and their advantages over current patient-reported outcomes
- Discuss high-dose home-exercise intervention provided via tele-rehabilitation with a focus on shoulder pain, function and strength of manual wheelchair users
- Identify novel approaches to evaluate myofascial pain syndrome
NIDRR-Sponsored ARRT Young Investigators Panel of Oral Presentations
FRI // 8:30 AM – 10:00 AM
| 8:30 AM – 8:45 AM | Functional Brain Activity After Memory Retraining in Traumatic Brain Injury: THE MEMREHAB TrialFaculty: Ekaterina Dobryakova, Kessler Foundation; Glenn Wylie, Kessler Foundation; Nancy Chiaravalloti, Kessler Foundation |
| 8:45 AM – 9:00 AM | Discharge From Acute Inpatient Rehabilitation: The Gap Between Physical and Cognitive Independence Achieved by TBI PatientsFaculty: Heather Glubo, Rusk Rehabilitation, NYULMC |
| 9:00 AM – 9:15 AM | The Complex Role of Bladder Management and Functional Mobility in Life Satisfaction for Individuals With Pediatric-Onset Spinal Cord InjuryFaculty: Alicia M. January, Marquette University |
| 9:15 AM – 9:30 AM | Response of School Districts to the New York State Concussion Awareness and Management Act: A Review of Implementation ProtocolsFaculty: Maria Kajankova, Mount Sinai Medical Center; Jennifer Oswald, Icahn School of Medicine at Mount Sinai; Lauren Terranova, Icahn School of Medicine at Mount Sinai; Anne Ambrose, Mount Sinai Medical School; Wayne Gordon, Mount Sinai School of Medicine |
| 9:30 AM – 9:45 AM | Measurement of Altered Muscle Properties in Stroke-Impaired Muscle Using Shear Wave Ultrasound ElastographyFaculty: Sabrina Lee, Northwestern University, Rehabilitation Institute of Chicago; Sam Speer, Rehabilitation Institute of Chicago; William Rymer, Rehabilitation Institute of Chicago |
| 9:45 AM – 10:00 AM | Geographic Variation in Functional Status Following Post-Acute Hip Fracture RehabilitationFaculty: Srinivas Teppala, University of Texas Medical Branch; Kenneth Ottenbacher, University of Texas Medical Branch; Amol Karmarkar, University of Texas Medical Branch; Amit Kumar, Preventive Medecine and Community Health, University of Texas Medical Branch; Soham Al Snih, University of Texas Medical Branch; James Graham, University of Texas Medical Branch; Timothy Reistetter, University of Texas Medical Branch |
NETWORKING BREAK // EXPO OPEN
PLENARY SESSION
Advances in Technology for Independent Living
FRI // 11:00 AM – 12:30 PM
Faculty
Geoff Fernie, BSc, PhD, MIMechE, CEng, PEng, CCE, Toronto Rehabilitation Institute, University Health Network, University of Toronto, Toronto, ON, Canada; Milos Popovic, PhD, Toronto Rehabilitation Institute, Toronto, ON, Canada; Alex Mihailidis, PhD, PEng, Toronto Rehabilitation Institute, Toronto, ON, Canada
Diagnosis/Area of Practice: Cross-Cutting
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
This session will focus on products that have been recently commercialized at TRI. Three senior scientists will present, including: Milos Popovic who will describe developments in the use of FES as a rehabilitation tool for stroke and spinal cord injury, Alex Mihailidis presenting recent advances in the application of robots for upper limb rehabilitation, and Geoff Fernie who will summarize several other advances in rehabilitation that have emerged from Toronto Rehab as new products recently. The session will conclude with a discussion of the commercialization strategies used by Toronto Rehab to achieve a high success rate in ensuring that our research has impact.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Become familiar with recent advances in treatment using advanced Functional Electrical Stimulation technology
- Become familiar with recent advances in affordable robots designed to assist with repetitive tasks in an upper limb clinic
- Describe rehabilitation technology advances at Toronto Rehab that are in the early stages of commercialization and will be available shortly to support practice
Geoff Fernie, BSc, PhD, MIMechE, CEng, PEng, CCE has a primary appointment at the University of Toronto as professor in the Department of Surgery with cross appointments that include the Institute of Biomaterials and Biomedical Engineering, Departments of Mechanical and Industrial Engineering, Physical Therapy, and Occupational Science and Occupational Therapy. He is a professional engineer and institute director for research at Toronto Rehabilitation Institute-UHN. Dr. Fernie is recognized as a world leader in the application of engineering to creating solutions for problems commonly encountered by people with disabilities. He is the principal investigator on a major infrastructure award from CFI which funded the most advanced design, prototyping and testing facilities for rehabilitation technology and assistive devices in the world. He is focused on the development of technology to help people continue to live in their own homes. He has 9 commercialized products and several currently in clinical trials. He has helped launch 4 successful companies. He has published over 141 peer reviewed journal papers and book chapters and has 22 awarded patents and an additional 13 filings. Most recently he was awarded the inaugural 2014 Honourable David C Onley Award by the Canadian Foundation for Physically Disabled Persons in recognition of his enormous contribution to the disability movement.
Milos R. Popovic, PhD received his PhD in mechanical engineering from the University of Toronto, Canada, and the Dipl. Electrical Engineer degree from the University of Belgrade, Serbia, He is the Toronto Rehab chair in spinal cord injury research. He is also a professor in the Institute of Biomaterials and Biomedical Engineering at the University of Toronto, and senior scientist and Neural Engineering and Therapeutics Team Leader at the Toronto Rehabilitation Institute, University Health Network. Both institutions are located in Toronto, Canada. In 2011, Dr. Popovic established the Centre for Research in Advanced Neural Implant Applications (CRANIA) at the University of Toronto. Dr. Popovic’s fields of expertise are functional electrical stimulation, neuroprostheses, neuro-rehabilitation, brain machine interfaces, modeling and control of linear and non-linear dynamic systems, robotics, and signal processing. His interests are in the areas of neuro-rehabilitation, physiological control systems, assistive technology, and brain machine interfaces. Dr. Popovic is also one of the co-founders of the Canadian National Spinal Cord Injury Conference, and the Advances in Neurorehabilitation Conference, which is part of the Festival of International Conferences on Caregiving, Disability, Aging and Technology, established in 2004 and 2007, respectively.
Alex Mihailidis, PhD, PEng is the Barbara G. Stymiest Research Chair in rehabilitation technology at the University of Toronto and Toronto Rehab Institute. He is also the graduate coordinator for the Clinical Engineering Program. He is an associate professor in the Department of Occupational Science and Occupational Therapy (U of T) and in the Institute of Biomaterials and Biomedical Engineering (U of T), with a cross appointment in the Department of Computer Science (U of T). He has been conducting research in the field of pervasive computing and intelligent systems in health for the past 15 years, having published over 150 journal papers, conference papers, and abstracts in this field. He has specifically focused on the development of intelligent home systems for elder care and wellness, technology for children with autism, and adaptive tools for nurses and clinical applications. He currently holds several major research grants from internationally recognized funding agencies to support this work (including both the Canadian and American Alzheimer Associations, NSERC, and CIHR). He is also a CIHR New Investigator. His research has been completed through collaborations with other researchers in this field from Canada, the United Kingdom, and the United States, and with various industrial partners.
ACRM SPECIAL INTEREST & NETWORKING GROUP MEETINGS
BI-ISIG Girls and Women with ABI Task Force Meeting
FRI // 12:30 PM – 1:45 PM
BI-ISIG: Long-Term Issues Task Force Meeting
FRI // 12:30 PM – 1:45 PM
Geriatric Rehabilitation Group Business Meeting
FRI // 12:30 PM – 1:45 PM
Communications Committee Meeting
FRI // 12:30 PM – 1:45 PM
Membership Committee Meeting (by invitation)
FRI // 12:30 PM – 2:00 PM
BI-ISIG: Disorders of Consciousness Task Force: Minimal Competency Guidelines for Rehabilitation of DOC Workgroup Meeting
FRI // 12:30 PM – 2:00 PM
LUNCH BREAK
FRI // 12:30 PM – 2:00 PM
LUNCH PROGRAMS
Keep learning, connecting, and earning CE credits right through lunch! Sponsored by ACRM Special Interest and Networking Groups, these onsite lunch programs feature renowned guest speakers and specialty topics and provide an ideal setting for connecting with like-minded colleagues.
Add a luncheon to your existing registration at any time by simply returning to online registration.
SPINAL CORD INJURY INTERDISCIPLINARY SPECIAL INTEREST GROUP (SCI-ISIG) LUNCHEON
with Speaker, Dr. Mark S. Nash
Fri // 12:30 PM – 2:00 PM
$ Ticketed event
Wellness After SCI: Are We Barking Up the Wrong Tree?
The presentation will address best practice approaches to foster physical wellness after SCI among stakeholders with injury, their caregivers, and health care providers. It will focus on why people with SCI may know the route to achieve physical wellness, but do not take the journey. In doing so, exploration of wellness barriers will be essential if the already established, evidence-based approaches to health attainment can be fully realized.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Define the multidimensional constructs of wellness.
- Identify component risks of cardiendocrine disease after SCI as a barrier to wellness.
- Explain guideline-driven approaches that would enhance physical wellness after SCI.
- Recognize barriers to wellness attainment in persons with SCI, their caregivers, and health care professionals.
Mark S. Nash, PhD, FACSM has centered his 29 years in academic medicine on evidence-based approaches to identifying and then managing early vascular disorders and cardiometabolic hazards for persons with spinal cord injuries. Much of his work examined exercise countermeasures to cardiometabolic component risks, including activity-based investigations of voluntary and FES-induced exercise. Dr. Nash served on multiple federal grant review panels for NIDRR, NIH, the CDC, and the VA, and is currently chair of the PVA Consortium for Spinal Cord Medicine panel charged with writing clinical practice guidelines for cardiometabolic diseases in persons with SCI.
30-MINUTE SYMPOSIA SERIES
FRI // 1:30 PM – 3:00 PM
Moderator: Virginia Mills, MS, PT, CCM, LicNHA, FACRM
1:30 PM – 2:00 PM: Deborah L. Wilkerson Early Career Award Lecture: Clinical Research in Pediatric TBI: An Early Clinical Investigator’s Experience and Lessons Learned
Presented by 2014 winner: Brad Kurowski, MD, MS
2:00 PM – 2:30 PM: Clinical Feasibility and Validity of the Kessler Foundation Neglect Assessment Process (KF-NAP) #1193
Faculty
Peii Chen, PhD; Kimberly Hreha, MS, OTR/L, Kessler Institute for Rehabilitation
Spatial neglect (SN) is a neurocognitive disorder prevalent in stroke survivors. Conventional neglect tests require challenge understanding the test results which can lead to missing symptoms. Therefore, we examined (1) the correlations between KF-NAP, the FIM and the BI and (2) the KF-NAP’s predictability in in-hospital safety and rehabilitation outcome. We prospectively recruited patients with unilateral stroke. The presence of SN was defined by KF-NAP score greater than zero. The results concluded that SN was present in approximately 70% of the participants, it predicted poorer functional independence even after longer length of stay, and provides valuable information as a rehabilitation outcome measure.
Learning Objectives
- To define spatial neglect
- To evaluate the significance of assessing for spatial neglect directly in patients’ activities of daily living
- To share the results of the multi-site, prospective, cohort study
2:30 PM – 3:00 PM: Exercise is Medicine and We Need to Prescribe in Conjunction With Comprehensive Lifestyle Counseling #1299
Faculty
Patricia Cristine Heyn, PhD, Colorado Intellectual & Developmental Disabilities Research Center (IDDRC), University of Colorado Denver Anschutz Medical Campus, Denver, CO; James Carollo, PE, PhD, Center for Gait and Movement Analysis, Children’s Hospital Colorado, University of Colorado Denver Anschutz Medical Campus, Denver, CO
This presentation will review and highlights some of the challenges and solutions for the physician providing lifestyle counseling, including basic and simple health promotion approached that could be easily incorporated into the clinical practice.
Learning Objectives
- Understand the significance of exercise and lifestyle counseling to health and the prevention and treatment of many chronic diseases
- Identify approaches to address physical activity and exercise in healthcare settings
- Learn how to implement a successful comprehensive health assessment and motivation program in the clinical practice
Evidence-Based Management of Secondary Conditions in Traumatic Brain Injury Inpatient Rehabilitation #1145
FRI // 2:00 PM – 3:30 PM
Faculty
Jennifer Bogner, PhD, FACRM, Ohio Regional TBIMS, Ohio State University, Columbus, OH; Ronald T. Seel, PhD, FACRM, Crawford Research Institute, Shepherd Center, Atlanta, GA; Susan D. Horn, PhD, Institute for Clinical Outcomes Research, Salt Lake City, UT; Flora M. Hammond, MD, FACRM, Indiana University School of Medicine, Rehabilitation Hospital of Indiana, Indianapolis, IN
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
In TBI inpatient rehabilitation, there are 4 common patient conditions that must be managed successfully to optimize both the utilization of rehabilitation services and functional outcomes: (1) insufficient nutritional intake; (2) medical conditions that may lead to acute rehospitalizations; (3) agitated behavior; and (4) patient engagement in the rehabilitation process. This symposium will describe the incidence, associated factors, and influence of these 4 conditions on rehabilitation lengths of stay and outcomes. This presentation will also identify evidence on effective interventions that improve these conditions and their influence on outcomes, and where possible, stratified evidence-based recommendations for their effective treatment.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the incidence, causes, interventions used, and duration of treatment for nutritional intake issues, their impact on outcomes, and those interventions that are most effective and under what circumstances
- Describe the incidence and causes of acute re-hospitalizations, associated factors, and practices that are most effective for reducing acute re-hospitalizations and under what circumstances
- Describe the incidence, duration, associated factors, and interventions used for agitation, and their association with outcomes
- Describe patient effort (engagement) in TBI rehabilitation therapies, the impact of age, severity and time on levels of effort, the association of effort to rehabilitation outcomes, and modifiable factors that influence effort in therapies
Pharmacotherapy of Post-Traumatic Cognitive Impairments: Investigations of Acetylcholinergic and Catecholaminergic Approaches #1287
FRI // 2:00 PM – 3:30 PM
Faculty
David B. Arciniegas, MD, Baylor College of Medicine, TIRR Memorial Hermann, Houston, TX; Thomas W. McAllister, MD, Indiana University School of Medicine, Indianapolis, IN
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This symposium will review the roles of acetylcholine, dopamine, and noradrenergic systems on cognition and the acute and chronic effects of TBI on these neurotransmitter systems. Studies of the cholinergic and catecholaminergic hypotheses of post-traumatic cognitive impairments performed by the presenters and their collaborators will be reviewed. Translation of findings from these studies into the design of several multicenter trials of medications post-traumatic cognitive impairments performed over the last decade will be discussed, and results of these clinical trials will be presented. Implications of this work on the development of effective treatments for post-traumatic cognitive impairments will be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Recognize the effects of traumatic brain injury on cerebral acetylcholinergic and catecholaminergic function
- Explain the cholinergic and catecholaminergic hypotheses of posttraumatic cognitive impairments and the evidence supporting them
- Describe cognitive deficits that are appropriate targets of acetylcholinergic and/or catecholaminergic medications
- Discuss medications for posttraumatic cognitive impairments and the evidence supporting them
Environment Matters: Contribution of Geographic Data to Understanding Spinal Cord Injury Incidence and Rehabilitation Outcomes #1231
FRI // 2:00 PM – 3:30 PM
Faculty
Yuying Chen, MD, PhD, University of Alabama at Birmingham, Birmington, AL; Amanda L. Botticello, PhD, MPH, Kessler Foundation, West Orange, NJ; Yue Cao, PhD, MSPH, Medical University of South Carolina, Charleston, SC
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Outcomes research
This symposium will review the conceptual and methodological approaches involving the use of geographic and administrative datasets for research in understanding environment and health. Examples will be provided from recent studies of spinal cord injury (SCI) incidence and rehabilitation outcomes to demonstrate the utilization of geocoding, census statistics, and geographic information system. Findings of geographic variation in outcomes associated with area-level differences, socioeconomic stratification, and the built environment will be discussed. The presentations will provide recommendations for the application of the study findings for clinicians seeking to maximize successful community living following SCI as well as future directions for research.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe conceptual and methodological approaches involving the use of large geographic and administrative datasets for research in understanding the environment and health
- Recognize the utilization of geocoding, census data, and geographic information system in spinal cord injury research
- Report community characteristics and their relation to spinal cord injury incidence and rehabilitation outcomes
- Discuss how the findings from current research can inform health care policy and guide clinical practice
Identifying and Addressing the Needs of Vulnerable Populations in Stroke #1181
FRI // 2:00 PM – 3:30 PM
Faculty
Barbara J. Lutz, PhD, RN, CRRN, APHN-BC, FAHA, FNAP, FAAN, School of Nursing, University of North Carolina-Wilmington, Wilmington, NC; Mary Ellen Young, PhD, College of Public Health and Health Professions, University of Florida, Gainesville, FL; Jill I. Cameron, PhD, University of Toronto, Toronto, ON, Canada; Linda L. Pierce, PhD, RN, CNS, CRRN, FAHA, FAAN, College of Nursing, University of Toledo, Toledo, OH; Victoria Steiner, PhD, University of Toledo, Toledo, OH; Stephanie Vaughn, PhD, RN, CRRN, School of Nursing, California State University, Fullerton, CA; Elaine Tilka Miller, PhD, RN, CRRN, FAHA, FAAN, College of Nursing, University of Cincinnati, Cincinnati, OH; Adelaide Harris, MSN, MEd, RN, College of Nursing, University of Cincinnati, Cincinnati, OH
Diagnosis/Area of Practice: Stroke
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Stroke occurs suddenly, causing significant residual impairment for stroke survivors requiring long-term assistance by family caregivers. Stroke is a leading cause of major disability worldwide. Several groups are disproportionately affected by stroke, including African Americans, Latinos, and family caregivers who are called upon to provide care for stroke survivors post-discharge. The focus of this symposium is to highlight the needs of vulnerable populations affected by stroke: African American women, Latino stroke survivors and caregivers, and family caregivers who find themselves overwhelmed by the new role, and discuss potential intervention strategies designed to meet the needs of these groups.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the needs of select vulnerable populations affected by stroke
- Review the overall state of the evidence underpinning interventions for these vulnerable populations
- Identify intervention strategies to meet the needs of these vulnerable populations
Pediatric Multiple Sclerosis: Cognitive, Fine Motor and Educational Impact #1221
FRI // 2:00 PM – 3:30 PM
Faculty
Maria C. Milazzo, RN, MS, Stony Brook University, Stony Brook, NY; Mary Squillace, DOT, OTR/L, Stony Brook University, Stony Brook, NY
Diagnosis/Area of Practice: Neurodegenerative disease (e.g., MS, Parkinson’s disease)
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Multiple Sclerosis (MS) is a multi-symptom disorder which targets the CNS. Nearly 5% of patients are diagnosed prior to age 18. Youth with MS face challenges of an unpredictable disease, with many “hidden symptoms,” including fine motor deficits and as many as 33% with cognitive impairment. Loss of time from school results in academic struggles and difficulty engaging with peers. This session will discuss the cognitive and psychosocial impact of Pediatric MS, barriers to educational accommodations and describe fine motor changes common to youth with MS. Recommendations for working in the clinical and educational settings will be provided.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe Pediatric onset Multiple Sclerosis
- Report the cognitive, psychosocial and fine motor implications of Pediatric Multiple Sclerosis
- Explain a brief evaluation battery that can be used in the clinical setting when assessing the motor skills of children with MS
- Discuss interventions for school programs and the barriers for accessing supportive accommodations in school
- Explore implications for further study
Pain Assessment and Management in Patients With Severe Brain Injury #1179
FRI // 2:00 PM – 3:30 PM
Faculty
Caroline Schnakers, PhD, University of California, Los Angeles, Los Angeles, CA; Camille Chatelle, PhD, Spaulding Rehabilitation Hospital, Boston, MA; John Whyte, MD, PhD, Moss Rehabilitation Research Institute, Elkins Park, PA
Diagnosis/Area of Practice: Pain
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Pain assessment in patients recovering from coma constitutes a real challenge as they cannot communicate the presence of pain and its subjective intensity. However, this is one of the most important topics to address as it has obvious clinical and ethical implications. This symposium will provide an overview of the current neuroimaging findings as regards pain perception in patients with disorders of consciousness and the recent development in behavioural protocols aiming to assess and treat pain in those patients.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the neural substrates linked to pain
- Target the difficulties to detect and manage pain in a clinical setting
- Become familiar with the tools available to assess pain in patients with disorders of consciousness
Improving Outcomes With Multimodal Prehabilitation in Surgical Cancer Patients #1149
FRI // 2:00 PM – 3:30 PM
Faculty
Julie K. Silver, MD, Harvard Medical School, Foxborough MA; Francesco Carli, MD, MPh McGill University; Daniel Santamina, PhD, University of Guelph-Humber, Toronto, ON, Canada; Ann Gamsa, PhD, Alan Edwards Pain Centre, McGill University Health Centre, Montreal. QC, Canada; Chelsia Gillis, MSc, University of Prince Edward Island, Charlottetown, PE
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Patients undergoing cancer surgery are at risk of delayed return to baseline functions. Prehabilitation aims to enhance physiological reserve preoperatively and therefore minimize the impact of the surgical stress response on the recovery process. This symposium will review the current knowledge and address the role of preoperative interventions in facilitating postoperative recovery.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify specific pathophysiologic responses to surgical stress in colorectal cancer patients
- Explain prehabilitation interventions that may reduce the pathophysiologic responses to stress in colorectal cancer patients
- Summarize the role of exercise, pre-operative nutritional assessments and interventions and relaxation to enhance peri-operative tolerance and post-operative recovery
Bridging the Gaps Between Medical Rehab and Schools for Students With Acquired Brain Injuries #1099
FRI // 2:00 PM – 3:30 PM
Faculty
Brenda Eagan Brown, MEd, CBIS BrainSTEPS Program, Brain Injury Association of Pennsylvania, Carlisle, PA; Drew A. Nagele, PsyD, CBIST, Beechwood NeuroRehab, Langhorne, PA; Brenda Eagan Brown, Brain Injury Association of Pennsylvania, BrainSTEPS Program, Carlisle, PA
Diagnosis/Area of Practice: Brain Injury/Stroke
Focus: Pediatric Rehabilitation
Each year, approximately 500,000 children in the U.S. experience a traumatic brain injury that dramatically impacts their ability to successfully perform in school. Another undetermined but likely significant number of children experience non-traumatic brain injuries such as stroke, tumors, seizure disorder, anoxic and metabolic disorders that also impact their school performance. The number one resource for children with acquired brain injury is their school. However, schools are ill equipped to tailor educational programming for children with cognitive and physical impairments following acquired brain injury. This symposium will describe an interventional approach to bridging the gaps between medical rehabilitation and schools.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify how students with acquired brain injuries needs are different from students with non-neurologic disabilities
- Describe best practices for school programming for students with ABI
- Identify steps that should be taken to form collaborative relationships between medical rehabilitation and school personnel
Longitudinal Outcome Models in Traumatic Brain Injury and Spinal Cord Injury: From Research to Practice #1107
FRI // 2:00 PM – 3:30 PM
Faculty
Allan J. Kozlowski, PhD, BSc (PT), Icahn School of Medicine at Mount Sinai, New York, NY; Kristen Dams O’Connor, PhD, Icahn School of Medicine at Mount Sinai, New York, NY; Marie-Christine Ouellet, PhD, École de psychologie, Université Laval, Centre interdisciplinaire de recherche en réadaptation et intégration sociale (CIRRIS), Québec QC; Jeffrey Cuthbert, PhD, MPH, MS, OT, Craig Hospital, Englewood, CO; Christopher R. Pretz, PhD, Craig Hospital, Englewood, CO
Diagnosis/Area of Practice: Brain Injury/Spinal Cord Injury
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Many important rehabilitation outcomes continue to change years after injury, yet common outcome assessment methods examine point-in-time events, such as at rehabilitation discharge. Researchers have begun to apply advanced longitudinal methods to facilitate understanding of individual progression of traumatic brain injury (TBI) and spinal cord injury (SCI) outcomes. This symposium will describe the application and interpretation of advanced longitudinal analyses in clinical and research settings. We demonstrate interactive tools to interpret individual-level change over time on the Extended Glasgow Outcomes Scale, the Disability Rating Scale, the Hospital Anxiety and Depression Scale, likelihood of employment, and the FIM™ Instrument Motor subscale.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe four types of longitudinal models: profile analysis, trend analysis, individual growth model analysis, and generalized linear mixed modeling
- Discuss the relevance, strengths, and limitations of using longitudinal models to evaluate rehabilitation outcomes
- Discuss clinical applications of longitudinal models for commonly used measures of physical, cognitive, emotional, and psychosocial functioning for persons with traumatic brain injury or spinal cord injury
- Use an interactive tool to construct various growth curves based on specific patient information
Environmental Factors Item Development for Persons with Stroke, Traumatic Brain Injury, and Spinal Cord Injury #1180
FRI // 2:00 PM – 3:30 PM
Faculty
Allen W. Heinemann, PhD, Center for Rehabilitation Outcomes Research, Rehabilitation Institute of Chicago, Northwestern University, Chicago, IL; Joy Hammel, PhD, OTR/L, University of Illinois at Chicago, Chicago, IL; Susan Magasi, PhD, University of Illinois at Chicago, Chicago, IL
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Environmental factors have a critical influence on participation; however, available instruments were not developed with contemporary measurement methods. Presenters will describe efforts to develop measures of environmental factors and define item sets of facilitators and barriers to participation following stroke, traumatic brain injury (TBI), and spinal cord injury (SCI). Instrument development included an extensive literature review, item classification and selection, item writing, and cognitive testing. Pilot testing involved adults with stroke, TBI, and SCI; testing with revised items involved 600 adults. Presenters will report the psychometric properties of the item banks and opportunities for utilization in research and clinical practice.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe methods used in operationalizing environmental factors
- Describe the results of a research project to develop measures of environmental factors that affect participation
- Define an initial item set of facilitators and barriers to participation following stroke, traumatic brain injury, and spinal cord injury
Preventing Cognitive Decline in Older Adults: Innovative Approaches #1176
FRI // 2:00 PM – 3:30 PM
Faculty
Deirdre Dawson, PhD, OT Reg (Ont), Rotman Research Institute, Baycrest, University of Toronto, Toronto, ON, Canada; Nicole Anderson, PhD, CPsych, Rotman Research Institute, Baycrest, University of Toronto, Toronto, ON, Canada; Kelly Murphy, PhD, CPsych, University of Toronto, Toronto, ON, Canada; Angela Troyer, PhD, CPsych, Baycrest, University of Toronto, Toronto, ON, Canada
Diagnosis/Area of Practice: Cross-Cutting/Geriatric Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Age-related cognitive decline is a serious personal and public-health problem with millions currently living with subjective cognitive complaints, Mild Cognitive Impairment (MCI) or dementia. Fortunately, research indicates age-related declines in functioning can be delayed through cognitive and lifestyle interventions. This symposia presents evidence regarding the benefits conferred from four unique programs targeting cognitive decline in seniors, focusing on normal age-related memory changes, age-related executive function changes, volunteering as a way to prevent physical, psychosocial and cognitive decline, and improving outcomes for people living with MCI.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Become familiar with the normal cognitive decline and cognitive decline indicative of mild cognitive impairment
- Gain knowledge regarding approaches to addressing cognitive decline for use with older adults with subjective cognitive complaints or mild cognitive impairment
- Consider the benefits of addressing cognitive decline through meaningful activity and/or contextualized practice of strategies
- Discuss clinical implications of programs presented and key directions for future research
The Role of Research in Reimbursement #1133
FRI // 2:00 PM – 3:30 PM
Moderator: Jennifer French, MBA, Neurotech Network, Tampa, FL
Faculty
Rachel E. Cowan, PhD, University of Miami Miller School of Medicine, Miami, FL; Scott Simcox, BE, MEE, PhD candidate, Restorative Therapies, Baltimore, MD; Chris Castel, PhD, Accelerated Care Plus Corp, a division of Hanger Inc, Reno, NV; Mary Schmidt-Read, PT, DPT, MS, SCI, Magee Rehabilitation, Philadelphia, PA; Anne Deutsch, PhD, BSN, Rehabilitation Institute of Chicago, Chicago, IL; Deborah Backus, PT, PhD, Shepherd Center, Atlanta, GA; Judy Murray, MPT, Mackenzie Health, Richmond Hill, ON, Canada
Diagnosis/Area of Practice: Cross-Cutting
Focus: Health/disability policy, ethics, advocacy
Out-of-pocket costs and third party reimbursement drive access to rehabilitation services, equipment, and technology for persons with neurological conditions. How can the research community impact clinical practice, clinical services and financial access? This panel discussion will focus on novel ways to collaborate with third party payers. It will also focus on how to provide research to support different reimbursement strategies. Open discussion with attendees will focus on developing relationships between clinicians and researchers to impact future outcomes and guide reimbursement decision making to support the consumer population.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the impact of the issues and perspectives of the consumer, clinician and industry in the reimbursement process providing financial access
- Provide examples of how research has impacted reimbursement for clinical services or equipment with successful outcomes
- Discuss novel ways to use research to gain access to essential services and equipment
- Strategize how to foster key relationships that promote rehabilitation research contributing to the reimbursement decision process
NETWORKING BREAK // EXPO OPEN
FRI // 3:30 PM – 4:00 PM
Best Practices in Concussion Management: Evidence for Rest, Exercise and Vestibular, Cognitive, and Emotional Rehabilitation #1200
FRI // 4:00 PM – 5:30 PM
Faculty
Jennifer V. Wethe, PhD, College of Medicine, Mayo Clinic in Arizona, Scottsdale, AZ; John J. Leddy, MD, University at Buffalo School of Medicine and Biomedical Sciences, Buffalo, NY; Rosemarie Scolaro Moser, PhD, ABN, ABPP-RP, Sports Concussion Center of New Jersey at RSM Psychology Center, LLC, Lawrenceville, NJ; Jamie M. Bogle, AuD, PhD, College of Medicine, Mayo Clinic in Arizona, Scottsdale, AZ
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Concussion has been described as a public health crisis, yet there is considerable variability and debate regarding the best management strategies. This symposium presents the scientific underpinnings and clinical research evidence for cognitive and physical rest versus exercise in the management of concussion and features two of the most prominent clinician-scientists on either side of the debate. The mechanisms of vestibular, cognitive, and emotional/behavioral dysfunction following concussion are reviewed and the techniques and evidence for rehabilitation of each are discussed. The symposium will conclude with a point-counterpoint discussion and synthesis of the evidence into clinical practice suggestions.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the utility and application of comprehensive rest in concussion treatment
- Describe the use of exercise testing for the evaluation of acute concussion and recovery and the use of individualized exercise treatment for post-concussion syndrome
- Identify the typical vestibular clinical presentation and recognize the use of vestibular rehabilitation in those with post-concussion syndrome
- Identify empirically supported treatments for the most common persisting cognitive deficits following concussion
Representation in the TBI Model Systems: Reflections From an Urban Model System #1278
FRI // 4:00 PM – 5:30 PM
Faculty
Tamara Bushnik, PhD, FACRM, Rusk Institute, NYULMC, New York, NY; Brian Im, MD, Rusk Institute, NYULMC, New York, NY; Yuliya Maystrvoskaya, DO, Rusk Institute, NYULMC, New York, NY; Heather Glubo, PhD, Rusk Institute, NYULMC, New York, NY
Diagnosis/Area of Practice: Brain Injury
Focus: Outcomes research/epidemiology
TBIMS hospitals have typically been academic medical centers, treating individuals that may not be representative of the larger population of individuals who sustain a TBI. In light of evidence of health disparities and the changing demographic profile of the US, particularly in urban areas, the demographic make-up of individuals receiving rehabilitation must be addressed to provide appropriate care. The Rusk Rehabilitation TBIMS (RRTBIMS) includes a hospital treating individuals regardless of ability to pay and is addressing the representativeness of vulnerable/minority groups and whether current research methods appropriately assess the heightened risks for poor health outcomes following TBI in these groups.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify how rehabilitation care may differ for individuals with TBI from minority or vulnerable populations
- Discuss the implications of health disparities in rehabilitation
- Examine the 72 hour inclusion criteria for the TBIMS and its implications in the representativeness of the TBIMS
Using Implementation Science: A Guide for Sustainable Practice Change in Spinal Cord Injury Rehabilitation #1161
FRI // 4:00 PM – 5:30 PM
Faculty
Cyndie Koning, PhD, OT (C), Glenrose Rehabilitation Hospital, Edmonton, AB, Canada; Laura Mumme, BSc, Alberta Health Services, Edmonton, AB, Canada; Dalton Wolfe, PhD, Lawson Health Research Institute, London, ON, Canada; Jacquie Brown, MES RSW, Jacquie Brown and Associates, Toronto, ON, Canada; Carol Scovil, PhD, Toronto Rehabilitation, UHN, Toronto, ON, Canada; Marie-Thérèse Laramée, MSc, BScPT, Institut de readaptation Gingras-Lindsay-de-Montreal, Montreal, QC, Canada; Kerry Bayless, BSc, Alberta Health Services, Edmonton, AB, Canada; Anna Kras-Dupuis, RN MScN, CNN(C), CRN(C), St. Joseph’s Health Care London, London, ON, Canada; Lynsey Hamilton, Rick Hansen Institute, Vancouver, BC, Canada; Magda Mouneimne, MScOT, Alberta Health Services, Foothills Medical Centre, Calgary, AB, Canada
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Implementation science is well recognized as the “missing link” between research-generated evidence and what actually happens in clinical practice. The Spinal Cord Injury Knowledge Mobilization Network is a collaboration of six Canadian rehabilitation centres that applied National Implementation Research Network active implementation frameworks to facilitate the implementation of two best practices in the area of pressure ulcer prevention in individuals with SCI. Monitoring and measuring both implementation processes and intervention outcomes are vital in determining whether evidence-based clinical practice is delivered as intended, and to examine impacts on patients and families.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Be introduced to the application of NIRN IS framework and the tools that may be used to move research to practice.
- Identify how to apply IS through examples from the SCI KMN work in pressure ulcer prevention.
- Clearly define core components of evidence based practice to facilitate implementation success.
- Describe how both implementation and outcome data are key drivers to improve practice through examples from the SCI KMN.
The Selective Tibial Neurotomy in the Treatment of the Spastic Equinovarus Foot Among Stroke Patients #1178
FRI // 4:00 PM – 5:30 PM
Faculty
Thierry Deltombe, MD, CHU Université Catholique de Louvain, Mont-Godinne, Yvoir Namur, Belgium
Diagnosis/Area of Practice: Stroke
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The selective tibial neurotomy (STN) is a neurosurgical procedure in which the motor nerve branches innervating the spastic muscles are partially sectioned. The STN can be performed at the level of the soleus, gastrocnemius, tibialis posterior, and flexor hallucis longus nerves. A previous diagnostic nerve block with anaesthetics helps to determine the nerve to treat and to predict the expected functional improvement. Uncontrolled longitudinal studies and a RCT have shown the long-lasting beneficial effect of the STN on spasticity, gait speed, and equinovarus deformity supporting the fact that STN should be considered as an option in the treatment of spastic equinovarus foot in hemiplegic patients.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Explain the neurotomy technique
- Explain the role of the diagnostic motor nerve block in the assessment of the spastic foot
- Review the scientific evidence of tibial neurotomy in the treatment of the spastic foot
- Discuss shown video cases of patients treated with neurotomy
Traumatic Brain Injury: Recovery and Decline #1269
FRI // 4:00 PM – 5:30 PM
Faculty
Robin E. A. Green, PhD, University of Toronto, University Health Network, Toronto, ON, Canada; Barbara Bendlin, PhD, University of Wisconsin School of Medicine and Public Health, Madison, WI; Jennifer C. Tomaszcyk, PhD, University Health Network, Toronto Rehab, Toronto, ON, Canada
Diagnosis/Area of Practice: Brain Injury/Neurodegenerative Diseases
Focus: Neuroscience (e.g., neural regeneration/repair, motor control/learning, biomechanics)
Moderate-severe traumatic brain injury has been long seen as a stable disorder in the chronic stages of injury. However, there is growing evidence that challenges this assumption. Research from the labs of the symposium speakers (and elsewhere) illustrates deterioration of the brain during the chronic stages of injury along with associated behavioural deterioration. This research also reveals the very large prevalence of the deterioration. Speakers will discuss these findings, along with their clinical implications. Finally, new research will be discussed that offers promise for offsetting neurodegeneration.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the reconceptualization of TBI as a chronic and progressive disorder
- Discuss research into clinical interventions to offset neurodegeneration
- Differentiate neuroimaging signs of neurodegeneration from signs of neural recovery
- Describe the evolution of depression the acute to the chronic stages of moderate-severe TBI
Applying the Biopsychosocial Model toward Prevention of Chronic Pain Syndrome #1289
FRI // 4:00 PM – 5:30 PM
Faculty
Virgil T. Wittmer, PhD, Brooks Rehabilitation, Jacksonville, FL; Steve Stanos, DO, Swedish Medical Center, Seattle, WA; Sara Bertoch, PhD, Rehabilitation Institute of Chicago, Center for Pain Management, Chicago, IL
Diagnosis/Area of Practice: Pain
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
We need to prevent acute/sub-acute pain from developing into chronic pain or a chronic pain syndrome. Early identification and treatment of biological, psychological and sociological risk factors are essential in this effort to avoid a dysfunctional response to pain. This approach mandates a true biopsychosocial perspective, as the traditional medical model approach has proven ineffective with this complex problem. This symposium will identify these risk factors, provide a variety of interdisciplinary assessments, and recommend interdisciplinary treatment strategies to prevent development of a chronic pain syndrome. Interdisciplinary rehabilitation is at the heart of this model of assessment and treatment.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Differentiate chronic pain from a chronic pain syndrome
- Understand the individual and social costs of chronic pain syndrome.
- Understand the biological, psychological, and social factors which contribute toward the development of a chronic pain syndrome
- Understand differential assessment and treatment strategies to provide within the first 3 months of pain onset in order to prevent development of a chronic pain syndrome
- Understand how an interdisciplinary biopsychosocial and rehabilitation approach is critical in the effort to prevent develop of a chronic pain syndrome
Disability Within the Context of Breast Cancer Screening, Treatment, and Survivorship #1285
FRI // 4:00 PM – 5:30 PM
Faculty
Robin Newman, OTD, OTR/L, University of Illinois at Chicago, Chicago, IL; Kathy Lyons, ScD, OTR/L, Geisel School of Medicine at Dartmouth College; Lebanon, NH; Susan Magasi, PhD, University of Illinois at Chicago, Chicago, IL
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This symposium will provide a framework for understanding the disability needs of women across the breast cancer care continuum from screening mammograms to participation-based interventions for women during the treatment and survivorship phases. We will discuss the impact of cancer on health, well-being, and participation as well as the impact of pre-existing disabilities upon cancer screening and treatment. We will highlight recent research designed to address disparities in screening and to develop broad, feasible rehabilitation interventions that reduce disability in breast cancer survivors.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe a framework for understanding the impact of cancer on health, well-being, and participation from screening through survivorship
- Discuss systems, policies and barriers to cancer screening among women with disabilities
- Discuss the unmet physical, social, emotional and cognitive needs of women along the cancer continuum from screening through survivorship
- Explain common participation restrictions among cancer survivors and evidence-based programs to address the participation needs of breast cancer survivors
- Discuss feasibility of evidence-based programs and models of delivery
School-Based Programs Promoting Symptom Resolution & Recovery for Concussion: REAP & BrainSTEPS CMT Models #1122
FRI // 4:00 PM – 5:30 PM
Faculty
Brenda Eagan Brown, MEd., CBIS, BrainSTEPS, Brain Injury Association of Pennsylvania, New Castle, PA; Karen McAvoy, PsyD, Center for Concussion, Rocky Mountain Youth Sports Medicine, Centennial, CO
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This concussion symposium highlights the multidisciplinary team approach to concussion, utilizing communication between medical/school/student/family to facilitate recovery. Implementing universal systemic collaboration among teams to maximize recovery within the first 4 weeks will be emphasized. The return to school progression and early academic adjustments that must occur will be discussed initially. The second half will focus on keeping students engaged at school by monitoring accommodations and maintaining implementation of cognitive rest while focusing on new learning throughout persistent symptoms. Colorado’s REAP concussion model and Pennsylvania’s BrainSTEPS: Concussion Return to School model will demonstrate how management can easily take place within the school.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the importance of working with other professionals through a multidisciplinary team to facilitate concussion recovery
- Identify appropriate return to school progression steps
- Recognize the impacts of a concussion on students K-12 in the classroom setting
- Pinpoint symptom-based academic adjustments and accommodations to manage both the acute and protracted recovery of concussion management at school
- Understand REAP and BrainSTEPS models and how they assist in creating the multidisciplinary team upfront on the systemic level to manage students concussions over time
Best Practices for Reporting Rehabilitation Research #1293
FRI // 4:00 PM – 5:30 PM
Faculty
Anne Deutsch, RN, PhD, CRRN, RTI International, Rehabilitation Institute of Chicago’s Center for Rehabilitation Outcomes Research, Chicago, IL; Linda Resnik, PT, PhD, Providence VA Medical Center, Brown University, Providence, RI; Holly DeMark, MPP, Center for Rehabilitation Outcomes Research, Rehabilitation Institute of Chicago, Chicago, IL; Kenneth J. Ottenbacher, PhD, OTR, Center for Rehabilitation Sciences, University of Texas Medical Branch, Galveston, TX
Diagnosis/Area of Practice: Cross-Cutting
Focus: Other
Published research manuscripts are frequently the only lasting product of a research study. If the manuscript lacks key details, readers may not be able to critically assess the strengths and weaknesses of the design, conduct, and analysis of the study. Reporting guidelines have been created for clinical trials (CONSORT), observational studies (STROBE), diagnostic accuracy studies (STARD), systematic reviews and meta-analyses (PRISMA), and other study designs. These guidelines assist authors, help reviewers and editors with the review process, and allow readers to critically appraise published manuscripts. During this symposium we will describe the purpose of reporting guidelines and review reporting guidelines.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the purpose and impact of reporting guidelines
- List 3 issues addressed in reporting guidelines
- List 3 types of studies that have reporting guidelines
Creating Change in Health Policy: Demonstrating the Value of Rehabilitation in the US and Canada #1291
FRI // 4:00 PM – 5:30 PM
Faculty
Gary R. Ulicny, PhD, Shepherd Center, Atlanta, GA; Deborah Backus, PT, PhD, Shepherd Center, Atlanta, GA; Gerben DeJong, PhD, FACRM, MedStar National Rehabilitation Network, Washington, DC; Judy Murray, PT, District Stroke Centre, Mackenzie Health, Toronto, ON, Canada
Diagnosis/Area of Practice: Cross-Cutting
Focus: Health/disability policy, ethics, advocacy
The symposium will focus on the use of evidence to design and use research to influence rehabilitation health policy. The presentation will focus on current health policy issues related to rehabilitation in the United States and Canada, a review of research and a future agenda for demonstrating the value of rehabilitation, and practical advice on implementing outcome measures into clinical practice across the rehabilitation continuum in order to provide data sets that can help to influence rehabilitation policy.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Understand the most critical rehabilitation issues facing the US and Canada.
- Develop an understanding of how research data can be used to influence public policy and what data is needed.
- Understand why demonstrating our value is critical to the future of rehabilitation.
- Learning how to design studies that demonstrate value and where are the gaps in our current knowledge base
- Discuss the role of the clinician in defining rehabilitation health policy, and utilizing standardized outcome measures to facilitate rehabilitation research in order to collect the best data to influence policy decisions
Novel Ways to Improve Mobility and Physical Function in Older Adults: A Targeted Intervention Approach #1198
FRI // 4:00 PM – 5:30 PM
Faculty
Jonathan Bean MD, MS, MPH, Spaulding Rehabilitation Network, Harvard Medical School, Boston, MA; Feng-Hang Chang, ScD, MPH, OTR, Health and Disability Research Institute, Boston University School of Public Health, Boston, MA; Gregory Hicks, PT, PhD, University of Delaware, Newark, DE; Jennifer Brach, PhD, PT, University of Pittsburgh, Pittsburgh, PA; Nancy Latham, PhD, Boston University, Boston, MA; Jessie VanSwearingen, PhD, PT, University of Pittsburgh, Pittsburgh, PA
Diagnosis/Area of Practice: Cross-Cutting/Geriatric
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Older adults fear losing their independence more than death. Mobility and physical function play a key role in maintaining independence. Historically, interventions to improve mobility and physical function in older adults have been only modestly successful. This symposium will provide an overview of current research projects aimed at identifying attributes related to impaired mobility and evaluating interventions designed to improve mobility and physical function in older adults with age, disease, and injury related impaired mobility and function.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Recognize the impact of impaired mobility and physical function on independence in older adults
- Identify contributors to impaired mobility and physical function in older adults such as pain, impaired timing and coordination of movement, decreased strength, and decreased endurance
- Gain familiarity with novel interventions to improve mobility and physical function in older adults
- Consider the nuances of developing and conducting an exercise intervention in older adults with age, disease, and injury related impaired mobility
Developing Outcomes Data Management and Reporting Capacity for Musculoskeletal Rehabilitation Programs #1288
FRI // 4:00 PM – 5:30 PM
Faculty
Allen W. Heinemann, PhD, Northwestern University Feinberg School of Medicine, Rehabilitation Institute of Chicago, Chicago, IL; Neil Segal, MD, MS, College of Medicine, College of Engineering, University of Iowa, Iowa City, IA; Jason H. Raad, PhD, Rehabilitation Institute of Chicago, Chicago, IL
Diagnosis/Area of Practice: Cross-Cutting
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
This symposium describes the results of a Foundation for Physical Medicine and Rehabilitation-funded project that selected common data elements (CDEs) for use by rehabilitation programs serving patients with musculoskeletal disorders. Rehabilitation programs can use CDEs in comparative effectiveness research, to describe patients and the outcomes they achieve, and compare programs’ outcomes and quality. CDEs were selected and features of a data management service were specified using a modified Delphi process. A panel of 29 technical experts and key informants assisted the project. This symposium will report the CDEs selected and the technical requirements for a musculoskeletal outcomes database.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the technical considerations related to implementing an outcomes data management system
- Utilize the ICF as an organizing framework for selection of CDEs
- Discuss an instrument selection strategy for target populations
- Describe the clinical expertise required to implement a data management system
Using Hip Fracture and Replacement Practice-Based Evidence Data to Transform Clinical Practice #1110
FRI // 4:00 PM – 5:30 PM
Faculty
Pamela Roberts, PhD, MSHA, OTR/L, SCFES, FAOTA, Cedars-Sinai Medical Center, Los Angeles, CA; Susan D. Horn, PhD, Institute for Clinical Outcomes Research, Salt Lake City, UT; Hilary Siebens, MD, Siebens Patient Care Communications, Seal Beach, CA; Harriet U. Aronow, PhD, Cedars-Sinai Medical Center, Los Angeles, CA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This symposium will provide an overview of Practice-Based Evidence (PBE) methodology including analytic challenges. The symposium will also provide an illustration of PBE variations in rehabilitation treatment for hip fracture treated with arthroplasty and discuss different patient recovery trajectories and strategies for transforming rehabilitation clinical practice through Clinical Practice Improvement (CPI). We will discuss how the findings from a PBE study on weight-bearing status during rehabilitation after arthroplasty for hip fractures can be used to facilitate translation of analytic findings through CPI in a rehabilitation setting.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Become familiar with practice-based evidence methodology including analytical challenges
- Increase awareness of hip fracture rehabilitation studies that utilized practice-based evidence to inform practice
- Describe strategies for how to utilize practice-based evidence to improve clinical practice
ACRM Membership Meeting
FRI // 5:45 PM – 6:30 PM
Henry B. Betts Awards Gala
Back to top
SATURDAY, 11 OCTOBER 2014
ACRM SPECIAL INTEREST & NETWORKING GROUP MEETINGS
BI-ISIG: Disorders of Consciousness Task Force: Acute Confusion Case Definition Workgroup Meeting
SAT // 7:00 AM – 8:30 AM
Program Committee Meeting (by invitation)
SAT // 7:30 AM – 8:30 AM
Health Policy Networking Group Meeting
SAT // 7:30 AM – 8:30 AM
[sm_hr]
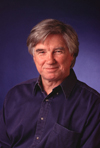 John Stanley Coulter Award Lecture: Improvements in Motor Function After SCI With Neuromodulation is Highly Dependent on Activity-Dependent Mechanisms
John Stanley Coulter Award Lecture: Improvements in Motor Function After SCI With Neuromodulation is Highly Dependent on Activity-Dependent Mechanisms
SAT // 8:30 AM – 9:30 AM
Presented by award winner, V. Reggie Edgerton, PhD
Dr. Edgerton is a distinguished professor of integrative biology and physiology and of neurobiology at the University of California, Los Angeles. His research is primarily focused on plasticity within the spinal neural networks that control motor function. Currently he is studying how epidural stimulation of the spinal cord in combination with pharmacological interventions can facilitate improvement in motor ability after spinal cord injury and other neurological injuries and diseases.
NETWORKING BREAK
SAT // 9:30 AM – 10:00 AM
Serving People With TBI and Addiction: Collaboration, Symbiosis, or Denial? #1137
SAT // 10:00 AM – 11:30 AM
Faculty
John D. Corrigan, PhD, Ohio State University, Columbus, OH; Carolyn M. Lemsky, PhD, Community Head Injury Resource Services of Toronto, North York, ON, Canada; Peter Selby, MD, Centre for Addiction and Mental Health (CAMH), University of Toronto, Toronto, ON, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Despite the high prevalence of co-morbid TBI and addiction, there has been very little communication, and even less collaboration, between providers in these service systems. In both fields, there is a paucity of research examining these co-occurring conditions. Complex psycho-social needs, stigma, and lack of awareness are all barriers to the development of practical and evidence-based models of care. This symposium will explore the relationship between substance misuse and TBI via current research projects conducted in addictions settings in the US and Canada. Recommendations for the management of substance use disorders in a rehabilitation context will be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the nature of the relationship between substance misuse and TBI, including risk factors for problematic substance use, and outcomes in rehabilitation and addictions settings
- Identify barriers to integrated care and the role of rehabilitation professionals
- Identify integrated models of care relevant for community and hospital based rehabilitation settings including Harm Reduction, Motivational Interviewing and Intensive Case Management
Use of Telemedicine in Spinal Cord Injury and Pressure Sore: A Pilot Project #1223
SAT // 10:00 AM – 11:30 AM
Faculty
Hilde Sørli, Sunnaas Rehabilitation Hospital, Nesoddtangen Akershus, Norway; Ingebjorg irgens, Sunnaas Rehabilitation hospital, Nesoddtangen Akershus, Norway; Gunnbjørg Aune, OT, Sunnaas Rehabilitation Hospital, Nesoddtangen Akershus, Norway; Hanne Haugland, Sunnaas rehabilitation Hospital, Nesoddtangen Akershus, Norway; Unn Svarverud, OT, Sunnaas Rehabilitation Hospital, Nesoddtangen Akershus, Norway
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Telemedicine is a promising outpatient approach for delivering pressure ulcer prevention and management to patients with SCI. We will describe the “Sunnaas Telerehabilitation Model,” as well as give a presentation of the telemedicine pilot project. The results from the project will be presented, and we will show how our pilot project has guided clinical out-patient practice at Sunnaas Rehabilitation Hospital. There are still clinical questions remaining to be solved, and further research is needed to obtain evidence-based practice. Some of these questions will be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the usefulness of telerehabilitation in terms of the right treatment, at the right location, at the right time
- Describe telemedicine as a promising approach for delivering pressure ulcer prevention and management to patients with SCI
- Describe the importance of multidisciplinary cooperation to succeed in using telemedicine in outpatient treatment
- Describe socioeconomic advantages by using telerehabilitation
- Demonstrate how current research can effectively guide clinical practice
Integration of Rehab Strategies and Surgical Reanimation for the Upper Limb After Stroke or SCI #1095
SAT // 10:00 AM – 11:30 AM
Faculty
Andrew Elkwood, MD, FACS, Center for the Treatment of Paralysis and Peripheral Nerve Surgery, Jersey Shore University Medical Center, Neptune, NJ; Neil Holland, MD, Neuroscience Institute, Monmouth Medical Center, Long Branch, NJ; Amy Bohn, CPAM, OTR/L, Children’s Healthcare of Atlanta, Atlanta, GA
Diagnosis/Area of Practice: Stroke/Spinal Cord Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Patients with central nerve system injuries, including stroke and spinal cord injuries, can regain function with nerve and tendon transfers. However, these patients have more complicated motor deficits than their counterparts with peripheral nerve injuries, because of spasticity and loss of reciprocal inhibition, with less predictable results from surgical reanimation. Although conventional electro diagnostic testing is usually not necessary for diagnostic purposes in these cases, unconventional techniques such as multichannel electromyography recording during movement can be very helpful to ensure a positive surgical outcome.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the role of electrodiagnositcs in the preoperative planning of the paralyzed patient
- Understand how the electro diagnostic examination for operative planning differs from that performed for diagnosis
- Discuss rehabilitation considerations before and after surgical intervention for reanimation
- Apply knowledge attained to discuss specific case examples of reconstructive and rehabilitative interventions in patients with both spastic and flaccid paralysis
Cognitive-Motor Interference in Persons With Parkinson’s Disease and Multiple Sclerosis #1183
SAT // 10:00 AM – 11:30 AM
Faculty
Lisa Muratori, PT, EdD, Stony Brook University, Stony Brook, NY; Jacob J. Sosnoff, PhD, University of Illinois at Urbana-Champaign, Urbana, IL; Joanne Wagner, PT, PhD, Saint Louis University, St. Louis, MO; John DeLuca, PhD, Kessler Foundation, West Orange, NJ
Diagnosis/Area of Practice: Neurodegenerative disease (e.g., MS, Parkinson’s disease)
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This course will examine cognitive-motor interference (CMI) in Parkinson’s disease (PD) and multiple sclerosis (MS). Presentations will focus on defining CMI, describing current evidence for unique interference characteristics in neurodegenerative diseases, assessment using dual task paradigms and potential intervention strategies. We will conclude with a brief question and answer session to engage attendees in this growing field of study and clinical practice.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Evaluate the importance of dual task assessment in persons with PD and MS
- Describe methods used to assess cognitive-motor interference in persons with PD or MS
- Discuss possible cognitive deficits revealed through dual task assessment in persons with PD or MS and describe current level of evidence for these deficits
- Discuss possible motor deficits revealed through dual task assessment in persons with PD and MS and describe current level evidence for these deficits
- Identify rehabilitation strategies to address cognitive-motor interference in persons with PD and MS
Interdisciplinary Pain Rehabilitation for Children and Adolescents #1173
SAT // 10:00 AM – 11:30 AM
Faculty
Gerard A. Banez, PhD, Cleveland Clinic Children’s Hospital for Rehabilitation, Cleveland, OH; Douglas Henry, MD, Cleveland Clinic Children’s Hospital for Rehabilitation, Cleveland, OH; Suzanne Daghstani, MS, OTR/L, Cleveland Clinic Children’s Hospital for Rehabilitation, Cleveland, OH
Diagnosis/Area of Practice: Pain
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This symposium will present an overview of interdisciplinary rehabilitation of children and adolescents with chronic pain and severe functional impairment. Following an introduction to pediatric chronic pain and its treatment, an interdisciplinary rehabilitation approach will be described. The roles and duties of medical, psychological, and rehabilitation specialists will be reviewed. The Cleveland Clinic Pediatric Pain Rehabilitation Program will then be presented as an example of an interdisciplinary pain rehabilitation program for chronic pain and severe functional impairment. Short-term and long-term outcomes of the program will be reviewed. Common clinical challenges and important research directions will be discussed.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe an interdisciplinary rehabilitation approach to pediatric chronic pain and distinguish this approach from an acute pain model
- Discuss the roles and duties of medical, psychological, and rehabilitation specialists in an interdisciplinary approach to pain rehabilitation for children and adolescents
- Describe the clinical outcomes associated with interdisciplinary pediatric pain rehabilitation and discuss common challenges
- Describe important research directions in pediatric pain rehabilitation
Rehabilitation of Medically Complex Liquid Tumor Inpatients: Challenges & Solutions #1241
SAT // 10:00 AM – 11:30 AM
Faculty
Jack B. Fu, MD, University of Texas, MD Anderson Cancer Center, Houston, TX; Arash Asher, MD, Cedars Sinai Medical Center, Los Angeles, CA; Kenley Schmidt, MD, Mayo Clinic, Rochester, MN
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Patients with hematopoietic malignancies are increased risk for medical complications. Rehabilitating liquid tumor inpatients in the setting of their medical fragility presents a number of challenges. Risk factors have been found to be associated with an increased risk of medical complications and several predictive models have been developed. Using this information can guide rehabilitation clinicians on the most appropriate inpatient rehabilitation setting. Another tool is mobile rehabilitation teams that provide an intense rehabilitation program while on the primary oncology service. This symposium will provide an overview of the strategies clinicians can use to rehabilitate these challenging patients.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify and discuss the kinds of medical complications experienced by cancer rehabilitation inpatients
- Discuss the published research on predictive risk factors for medical complications in this population
- Identify ways to use these predictive risk factors in the rehabilitation decision making process
- Discuss rehabilitation models to minimize medical complications and disruption of rehabilitation
What is Unique About Military and Veteran Rehabilitation After Brain Injury? #1184
SAT // 10:00 AM – 11:30 AM
Faculty
Risa Nakase-Richardson, PhD, James A. Haley Veterans Hospital, Tampa, FL; Jacob Kean, PhD, VA HSR&D Center for Health Information and Communication, Richard L. Roudebush VA Medical Center, Indianapolis, IN; Treven Pickett, PsyD, ABPP, VA Advanced Fellowship in Mental Illness Research and Treatment, Hunter Holmes McGuire VA Medical Center, Richmond, VA; Joel Scholten, MD, Washington DC VA Medical Center, Washington, DC; James F. Malec, PhD, Indiana University School of Medicine, Rehabilitation Hospital of Indiana, Indianapolis, IN; Chris MacDonell, Medical Rehabilitation and International Aging Services/Medical Rehabilitation, CARF International, Washington, DC
Diagnosis/Area of Practice: Brain Injury, Veteran and Military Populations
Focus: Outcomes research/epidemiology
Programs and practices developed for persons with moderate to severe TBI have been adapted for recent veterans with traumatic brain injury (TBI). The primary purpose of this symposium is to consider the degree to which current studies of service needs and outcomes conducted within the VA Polytrauma System of Care support differentiation of military and private rehabilitation program structures. New findings will be reported and serve as a backdrop for a discussion of rehabilitation program structures and a newly initiated CARF effort to ensure standards address the needs of service members and Veterans with TBI and persistent post-deployment symptoms.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Detail conceptual and practical differences between VA/DoD and private rehabilitation program structures
- Discuss potential drivers of differences in participation of Veterans with TBI
- Describe the integration of multiple sources of data to identify persons with emergent or ongoing rehabilitation needs
- List differences in outcomes between VA and NIDRR TBI Model System programs
- Debate the need for a unique rehabilitation program structure to serve current conflict veterans with TBI
An Interdisciplinary Clinical Practice Guideline for Concussion Management: Translating Evidence into Practice #1207
SAT // 10:00 AM – 11:30 AM
Faculty
Cristin Beazley, PT, DPT, Sheltering Arms Rehabilitation Centers, Mechanicsville, VA; Laura Brach, PT, DPT, Sheltering Arms Rehabilitation Centers, Mechanicsville, VA; Christy Littaua, MD, Sheltering Arms Rehabilitation Centers, Mechanicsville, VA; Anthony Melchiorre, Jr., PsyD, Sheltering Arms Rehabilitation Centers, Mechanicsville, VA; Anne Chan, PT, DPT, MBA, NCS, Sheltering Arms Rehabilitation Centers, Mechanicsville, VA
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The continued development and implementation of concussion management services is necessary to address the current state of assessment and treatment in this clinical area. Growing evidence coupled with improved diagnostic and treatment protocols and overall increased prevalence of concussion diagnoses have demonstrated the need for multi-disciplinary clinical management. This symposium will describe a clinical practice guideline for concussion management and delineate the multi-disciplinary model of care.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the importance of a clinical practice guideline for evidence in translation in concussion management
- Describe the roles of PT, PM&R and psychology in a concussion management program
- Evaluate current evidence for effective PT management of concussion
- Identify when it is appropriate to refer to PM&R and psychology for concussion management
- Become familiar with the business and operational aspects of a PT-led concussion management program
Exploring Frontiers in Rehabilitation Science & Technology #1283
SAT// 10:00 AM – 11:30 AM
Faculty
Fabrisia Ambrosio, PT, PhD, University of Pittsburgh, McGowan Institute for Regenerative Medicine, Pittsburgh, PA; Jeffrey Kleim, PhD, Arizona State University, Tempe, AZ; Edelle Field-Fote, PhD, PT, University of Miami Miller School of Medicine, Coral Gables, FL
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
The development and translation of innovative medical technologies has the potential to dramatically impact the future of rehabilitation practice. In this symposium, we will overview the state-of-the-science of three such technologies: regenerative medicine, genomics, and non-invasive brain stimulation, and highlight opportunities for integration with rehabilitation clinical practice and research initiatives.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the objectives and approaches of regenerative medicine and identify the highlight the future value of increasing regenerative medicine-rehabilitation interfaces (i.e., Regenerative rehabilitation).
- Describe how genomics can influence the capacity for neural plasticity and inform neurorehabilitation.
- Explain how neural activation via non-invasive brain stimulation activates neuroplastic mechanisms that can augment the effects of motor training.
- Promote an interactive discussion regarding the challenges to the incorporation of rehabilitation into the development of innovative medical technologies as well as methods to address these challenges.
Exoskeleton-Assisted Walking for Persons With Neurological Conditions, Part I: The State of the Science #1108
SAT // 10:00 AM – 11:30 AM
Faculty
Allan J. Kozlowski, PhD, BSc (PT), Icahn School of Medicine at Mount Sinai, New York, NY; Ann M. Spungen, EdD, Icahn School of Medicine at Mount Sinai, New York, NY; Candy Tefertiller, PT, DPT, ATP, NCS, Craig Hospital, Englewood, CO; Gail F. Forrest, PhD, Rutgers New Jersey Medical School, The State University of New Jersey, Newark, NJ; Clare Hartigan, PT, MPT, Virginia C. Crawford Research Institute, Shepherd Center, Atlanta, GA; Nicholas Evans, MHS, ACSM-CES, Beyond Therapy, Virginia C. Crawford Research Institute, Shepherd Center, Atlanta, GA; Arun Jayaraman, PT, PhD, Max Nader Center for Rehabilitation Technologies & Outcomes Research, Rehabilitation Institute of Chicago, Chicago, IL
Diagnosis/Area of Practice: Cross-Cutting
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
Powered exoskeletons offer persons with lower extremity paralysis and weakness due to neurological conditions opportunities to reengage in walking as a routine activity. Researchers have begun exploring the effects of exoskeleton-assisted walking for persons with spinal cord injury, traumatic brain injury, and stroke using three exoskeleton models. This symposium will describe the walking protocols, participant characteristics, mobility results, and concurrent changes to secondary conditions such as body composition, pain, spasticity, bowel function, and other aspects of quality of life observed in four independent research settings. The presenters will synthesize results from six independent studies and recommend directions for future research.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify four characteristics that distinguish currently available powered exoskeletons from antecedent technologies
- Describe five key components of instruction protocols for exoskeleton-assisted walking for persons with spinal cord injuries
- Discuss the relevance of personal and injury/condition characteristics of persons who have demonstrated ability to walk with one or more of three powered exoskeletons
- Describe improvements in four secondary conditions of SCIs reported for early exoskeleton-assisted walking trials
Oral Presentation of Scientific Papers — Stroke/Stroke-Related Topics
SAT // 10:00 AM – 12:00 PM
Moderator: Julie Haarbauer-Krupa, PhD
10:00 – 10:20: A Multi-Center Randomized Controlled Trial of Pediatric Constraint-Induced (P-CIMT) Movement Therapy (#2002)
Presented by Stephanie DeLuca
10:20 – 10:40: Modeling the Link Between Structural Connectivity Network Disruption and Performance and Activity Limitation in Stroke (#1806)
Presented by Amy Kuceyeski
10:40 – 11:00: Is Unstructured Peer Support After Stroke Sufficient to Improve Quality of Life? (#1929)
Presented by Laurien Aben
11:00 – 11:20: The effect of an arm supporting training device in sub-acute stroke patients: Randomized Clinical Trial (#1950)
Presented by Johan Rietman
11:20 – 11:40: Delivery Of Constraint-Induced Movement Therapy Through A Video Game: a Pilot Study in Stroke (#1652)
Presented by Lynne Gauthier
Oral Presentation of Scientific Paper — Mixed Topics
SAT // 10:00 AM – 12:00 PM
Moderator: Chris MacDonell
10:00 – 10:20: Comparison of the OPUS and FOTO’s Functional Status Measures for Persons with Lower Limb Amputation (#1653)
Presented by Alex Wong
10:20 – 10:40: How Should We Measure Participation in Older Adults? An Analysis from Boston RISE (#1748)
Presented by Marla Beauchamp
10:40 – 11:00: Pilot Testing a Positive Psychology Intervention in Individuals with Chronic, Disability-related Pain (#1635)
Presented by Rachel Müller
11:00 – 11:20: Long-term Functioning of Patients With Aneurysmal Subarachnoid Hemorrhage: a 4-year Follow-up Study (#1718)
Presented by Wendy Boerboom
11:20 – 11:40: An Efficient Method for Assigning Neurorehabilitation Outpatients to Treatment (#1741)
Presented by Hilary Bertisch
20. INSTRUCTIONAL COURSE:
Multidisciplinary Approach in the Management of Sports Concussion
SAT // 10:00 AM – 2:00 PM
Faculty
Angela Yi, PhD; Tricia Kasamatsu, MA, ATC, Certified Athletic Trainer; Vernon Williams, MD; Jose Posas, MD; Sports Concussion Institute, Anaheim, CA
Diagnosis/Area of Practice: Brain Injury. Also relevant to pain rehabilitation.
Focus: Clinical Practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Clinicians
Traumatic brain injuries sustained in sports have received increased nationwide public attention and there is a growing need for clinicians to be trained in the management of sports concussions. A sports related concussion can result in physical, cognitive, and emotional symptoms and requires a multidisciplinary network of healthcare providers who understand the various facets of sports concussion management that include prevention, assessment, diagnosis, intervention, follow-up care, and education. This instructional course will provide an overview of sports concussion management that will translate evidence and consensus-based guidelines into clinical practice and incorporate a multidisciplinary team approach to managing sports concussion.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- To learn foundational information regarding the epidemiology, pathophysiology, and symptoms, of a sports related concussion.
- To receive an overview of the various components that comprises a comprehensive sports concussion management program.
- To understand the various roles members of a multi-disciplinary team would serve in managing a sport related concussion and post-concussion syndrome.
- To explore the role of telemedicine in the delivery of sports concussion management.
21. INSTRUCTIONAL COURSE:
Physician Investigator Basic Training
SAT // 10:00 AM – 2:00 PM
Faculty
Sue Ann Sisto, PT, MA, PhD, FACRM, Stony Brook University, Stony Brook, NY; Flora Hammond, MD, Indiana University, Rehabilitation Hospital of Indiana, Indianapolis, IN; Mike Jones, PhD, Shepherd Center, Atlanta, GA; Ismari Clesson, RN, Shepherd Center, Atlanta, GA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Intended Audience: Physicians, nurses, therapists, and other healthcare professionals involved in or interested in clinical research.
The purpose of this course is to assist new physician investigators and key research staff in improving their skills and understanding of the principles and practices used in the successful execution of patient-oriented research. Participants will gain insights to enhance their ability to perform qualify research according to existing regulations and guidelines. The course is open to physicians, nurses, therapists, and other healthcare professionals involved in or interested in clinical research. The program will share information and create an opportunity for dialogue amongst attendees and program faculty.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe the current landscape of clinical research and opportunities for the physician investigator
- Discuss issues in the design, conduct, and management of successful clinical research studies
- Discuss investigator responsibilities related to regulations and ethics
- Describe avenues for dissemination and collaboration
22. INSTRUCTIONAL COURSE:
Ensuring the Delivery of High-Quality Fall Prevention: How Rehabilitation Professionals Engage in Quality Improvement
SAT // 10:00 AM – 2:00 PM
Faculty
Anne Deutsch, PhD, RTI International, Northwestern University Feinberg School of Medicine, Chicago, IL; Natalie E. Leland PhD, OTR/L, BCG, FAOTA, University of Southern California, USC Davis School of Gerontology, Los Angeles, CA; Pamela Roberts, PhD, MSHA, OTR/L, SCFES, FAOTA, CPHQ, Cedars-Sinai Medical Center, Los Angeles, CA; Jennifer C. Sidelinker, PT, DPT, GCS, Genesis Rehab Services, Kennett Square, PA
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Intended Audience: Rehabilitation clinicians, administrators, and provider organizations engaging in quality improvement initiatives and facilitating the translation and implementation of evidence into the clinical setting.
The translation and implementation of evidence into practice and an organization’s continuous quality improvement are pivotal for reducing the occurrence of poor patient outcomes – imperative in the era of the Affordable Care Act (ACA). Using a rehabilitation relevant to the adverse event of accidental falls as an exemplar, this symposium will provide an overview of how rehabilitation professionals and administrators can collaborate in the provision of high-quality care. Evidence and practice examples will be discussed in the context of ACA value-based payment, quality improvement, and implementation science, to equip participants with tools to enhance quality improvement initiatives in their practice setting.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe current fall prevention evidence for in-hospital and post-acute care rehabilitation patients
- Discuss the role of value-based purchasing in the context of rehabilitation service delivery
- Identify the theoretical constructs that support the translation and implementation of evidence into practice
- Verbalize the key components of continuous quality improvement
Sex Differences in Comorbidities After Neurotrauma: Implications for Rehabilitation #1256
SAT // 12:30 PM – 2:00 PM
Faculty
Angela Colantonio, PhD, OT Reg. (Ont.), FACRM, University of Toronto, Toronto Rehabilitation Institute, Toronto, ON, Canada; Vincy Chan, MPH, PhD Candidate, University of Toronto, Toronto Rehabilitation Institute, Toronto, ON, Canada; Heather B. Taylor, PhD, TIRR Memorial Hermann, Houston, TX; Susan Robinson-Whelen, PhD, TIRR-Memorial Hermann, Houston, TX; Yelena Goldin, PhD, JFK Johnson Rehabilitation Institute, Edison, NJ; Tara Jeji, MD, MBA, Ontario Neurotrauma Foundation, Toronto, ON, Canada
Diagnosis/Area of Practice: Spinal Cord Injury/Brain Injury
Focus: Outcomes research/epidemiology
Neurotrauma is more common than breast cancer, HIV/AIDS, and multiple sclerosis combined. There has been extensive research on neurotrauma and comorbidities, however, there is currently a paucity of research that considers sex and gender differences among those with spinal cord injury (SCI) and traumatic brain injury (TBI). This symposium will focus on sex and gender differences in comorbidities. It will begin with findings from a recent a systematic review, followed by three presentations on TBI and SCI using large datasets. This symposium will conclude with a session from the perspective of an individual with lived experiences.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe and discuss sex differences in medical and psychiatric outcomes after traumatic brain injury and sex-specific diagnostic and treatment considerations from a systematic review
- Describe and identify sex differences in the characteristics, outcomes, and comorbid health conditions of women and men with traumatic brain injury in inpatient rehabilitation from a publicly insured healthcare system
- Identify and recognize differences in comorbidities and secondary conditions among men and women with spinal cord injury
- Discuss sex differences and comorbidities from the perspective of a person with lived experiences
- Identify depression as a serious secondary condition for men and women with SCI and the treatment implications for women with SCI
Skeletal Muscle Adaptations Following Spinal Cord Injury and Their Impact on Establishing Appropriate Interventions #1286
SAT // 12:30 PM – 2:00 PM
Faculty
Ceren Yarar-Fisher, PT, PhD, University of Alabama at Birmingham, Birmingham, AL; C. Scott Bickel, PT, PhD, University of Alabama at Birmingham, Birmingham, AL; Kevin McCully, PhD, University of Georgia, Athens, GA; Elizabeth Sasso, PT, PhD, Shepherd Center, Atlanta, GA
Diagnosis/Area of Practice: Spinal Cord Injury
Focus: Other
While today individuals with spinal cord injury (SCI) tend to live much longer than in past decades, the protracted life expectancy is associated with increased risk of cardio-metabolic disease. This increased disease risk has been linked to the changes in skeletal muscle phenotype and metabolism after SCI. The aim of this symposium is to describe skeletal muscle adaptations following SCI and discuss how training via electrical stimulation can positively impact these adaptations. In addition, a roundtable discussion on the role of muscle physiology to guide and assist clinician will be held at the end of presentations.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss skeletal muscle adaptations to spinal cord injury
- Describe how electrical stimulation influences skeletal muscle vasculature and metabolism after spinal cord injury
- Describe the effects of contractile activity on skeletal muscle signaling pathways associated with glucose utilization
- Discuss how neuromuscular electrical stimulation training can be utilized to improve the impaired metabolic state in individuals with long term spinal cord injury
- Discuss the role of muscle physiology to guide and assist clinicians
What Did We Learn From the Longitudinal Studies on Aging and Cognitive Function? #1297
SAT // 12:30 PM – 2:00 PM
Faculty
Patricia Cristine Heyn, PhD, Colorado Intellectual & Developmental Disabilities Research Center (IDDRC), University of Colorado Denver Anschutz Medical Campus, Denver, CO
Diagnosis/Area of Practice: Stroke/Neurodegenerative Diseases
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
This presentation will discuss the research that differentiates between normal and pathological aging with considerations to the evidence on healthy aging and cognitive function outcomes. In addition, the role of longitudinal studies in assessing the rate of cognitive decline and the differences in rates of decline will be discussed. Finally, attention will be given to the role of longitudinal studies in the early detection of risk for dementia.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Gain knowledge about the importance of early detection of cognitive decline and how it is becoming more important for treatment and long-term planning
- Understand the distinction between mild cognitive impairment and dementia and the challenges for the clinician in recognizing memory loss in the rehabilitation patients
- Identify cognitive and functional measurements that could help identify the early signals of cognitive decline
- Recognize signals indicating the transition from normal cognitive aging to MCI and early dementia
Goal Setting in Rehabilitation: Theory, Practice and Evidence #1202
SAT // 12:30 PM – 2:00 PM
Faculty
Richard J. Siegert, BSc, PGDipPsych(Clin), MSocSci, PhD, Auckland University of Technology, Auckland, New Zealand; William M. M. Levack, BPhty, MHealSc(Rehabilitation), PhD, University of Otago, Wellington, New Zealand; Kathryn M. McPherson, BA(Hons), DipHV, RN, RM, FAFRM (Hons), PhD, Auckland University of Technology, Auckland, New Zealand; Sue Sherratt, BA, GCTT, BA (Speech Pathology and Audiology) Hons, PhD, University of Queensland, Australia
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Goal setting is considered one of the cornerstones of contemporary rehabilitation practice, yet the scientific foundations of goal setting in rehabilitation have, at least up until recently, been tenuous at best. The aim of this symposium is to provide clinicians and researchers with a state-of-the-art overview of rehabilitation goal setting. The symposium will focus on: (i) the theoretical basis for goal setting, (ii) the current best evidence underpinning goal setting practice, and (iii) clinical and applied aspects of goal setting, with specific attention to the moral dimensions of practice and to goal setting for people with aphasia and their families.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Provide an overview of the current best evidence for goal setting as a means of improving outcomes in rehabilitation
- List the major psychological models used to underpin goal setting in rehabilitation and identify some emerging models
- Report how to apply goal setting in specific rehabilitation contexts, including setting meaningful goals with individual adults in neurological rehabilitation and goal setting with adults with aphasia (and their families and clinical teams)
- Discussion and critique bioethical consideration in the application of goal setting to clinical practice
Conducting Clinical Research in an Outpatient Pain Management Practice Setting; Benefits and Challenges #2082
SAT // 12:30 PM – 2:00 PM
Faculty
Joan Cutillo, LPN, CCRC, National Pain Research Institute, LLC, Orlando, FL; Alexander Jungreis, MD, National Pain Institute, National Pain Research Institute, LLC, Orlando, FL; Cherian K. Sajan, MD, National Pain Research Institute, LLC, Orlando, FL
Diagnosis/Area of Practice: Pain
Focus: Research methods (e.g., measurement, research design analytic/statistical methods)
Treating the chronic pain patient is a daily challenge for success. The variables involved in the treatment decision making process are numerous and the medicinal treatment options are dwindling. Interventional physicians can overcome some of these challenges and actually benefit from including clinical trials in their pain management practice. There is a need for clinical trials in every community, especially in the chronic pain patient. It opens avenues for treatment that would not have been available without the trial. Many other diagnostic and financial benefits can result from a pain practice’s involvement in research and this information needs to be offered to practitioners.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify and train the best staff for a successful research team
- Recognize the proper study for their facility through feasibility study criteria and patient base
- Negotiate a profitable but fair contract and budget and invoice management
- Identify and overcome challenges of integrating daily activities of a research practice with a clinic practice
Post-Mastectomy Pain Syndrome: Etiology and Risk Factor Identification Informs Current and Future Treatment Options #1121
SAT // 12:30 PM – 2:00 PM
Faculty
Eric Wisotzky, MD, Medstar National Rehabilitation Hospital, Georgetown University School of Medicine, Washington, DC; Susan Maltser, DO, Hofstra North Shore-LIJ School of Medicine, Hempstead, NY; Yvonne Francis, PT, MBA, CLT, Medstar National Rehabilitation Hospital, Howard University School of Physical Therapy, Washington, DC
Diagnosis/Area of Practice: Cancer Rehabilitation
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Post-mastectomy pain syndrome (PMPS) is a complication of breast cancer treatment with prevalence of approximately 25%-60%. There are many possible etiologies of this pain syndrome. A specific diagnosis will lead to more effective treatment. Biomechanical research on the changes in shoulder mechanics after breast cancer treatment will be presented. Current research on the management of PMPS will be discussed. Identification of risk factors for PMPS may aid in the early identification and prevention of this pain syndrome. Research on risk factors for PMPS will be discussed, including findings on the role of psychological risk factors.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Identify common etiologies of post-mastectomy pain syndrome
- Recognize common risk factors for the development of post-mastectomy pain syndrome
- Cite a reasonable treatment approach to post-mastectomy pain syndrome
Interprofessional Development to Support the Transition of Students With TBI From Postsecondary Education to Employment #1242
SAT // 12:30 PM – 2:00 PM
Faculty
Eileen Elias, Med, Disability Services Center, JBS International, Inc, North Bethesda, MD
Diagnosis/Area of Practice: Brain Injury
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
Individuals with TBI often experience long-term cognitive impairments, including deficits with short-term memory, leading to barriers in gaining and maintaining employment. In a 5-year Project Career development, Kent State University, West Virginia University, Boston University, and JBS International will merge assistive technology and vocational rehabilitation best practices to support veteran and civilian postsecondary students with TBI transition to employment. This symposium will describe the best practices models utilized in this project, including the Matching Person and Technology Model, outcomes and lessons learned for year one.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe barriers individuals with TBI face in transitioning from education to employment settings
- Explain the importance of technology, including cognitive support technology, in helping individuals with TBI to perform daily tasks and succeed in academic and employment settings
- Describe the Project components and best practices models used to provide effective support and services, including the Matching Person and Technology Model
- Provide an overview of Project Career activities as well as outcomes and lessons learned one year since inception of the program
Neurosexuality: Neurobehavioral Approaches to the Study of Sexuality After Traumatic Brain Injury #1135
SAT // 12:30 PM – 2:00 PM
Faculty
Jhon Alexander Moreno, MSc, University of Montreal, Montréal, QC, Canada; Caron Gan, RN, MScN, Holland Bloorview Kids Rehabilitation Hospital, Toronto, ON, Canada; Nathan Zasler, MD, Tree of Life and Concussion Care Centre of Virginia, Ltd, Richmond, VA; Michelle McKerral, PhD, Université de Montréal, Montreal, QC, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Neurosexuality is the scientific study of the relationships between sexuality and the brain. Traumatic Brain Injury (TBI) is an example of the disruption of different neurological systems that affect sexuality with 50 to 60% of individuals with TBI reporting some level of sexual difficulties post injury. This inter-disciplinary symposium will introduce a biopsychosocial approach to assessment and intervention post TBI, highlighting the interplay between medical and physical issues, neuropsychological and psychological effects, and relationship factors. These topics will provide insight into the complexity of sexual concerns following TBI, shedding light into both clinical and research needs of individuals with TBI.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Illustrate neurosexuality through the relationship between neurological aspects and sexuality following TBI
- Introduce a biopsychosocial framework to conceptualize sexual difficulties after TBI
- Describe an interdisciplinary approach to addressing medical and physical issues, neuropsychological and psychological effects, and relationship factors influencing sexuality after TBI
- Summarize findings and recommendations regarding sexuality and psychosexual dysfunction after TBI
Innovative Assessments and Treatments in Cognitive Rehabilitation #1185
SAT // 12:30 PM – 2:00 PM
Faculty
Nancy D. Chiaravalloti, PhD, Kessler Foundation Research Center, West Orange, NJ; Yael Goverover, PhD, OT, New York University, New York, NY; Denise Krch, PhD, Kessler Foundation Research Center, West Orange, NJ; Carolina Bottari, PhD, OT, Université de Montréal, Montreal QC, Canada
Diagnosis/Area of Practice: Brain Injury
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
The primary aim of cognitive rehabilitation is to help individuals with cognitive impairments restore or compensate for cognitive deficits. Assessment of cognitive rehabilitation outcomes varies from traditional assessments of cognitive domains to self-reported assessment of global functioning. The aim of this symposium is to present new evidence regarding the use of contemporary assessment and treatment approaches designed for use with individuals who have cognitive impairment. We will present an innovative functional assessment, using the internet to assess cognitive processes. We will also present three new treatment protocols which represent a spectrum of cognitive rehabilitation approaches, from remedial to functional.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Discuss the cognitive deficits in TBI and their association with various activities of daily living
- Describe the modified Story Memory Technique and the results of a clinical trial with participants with TBI
- Identify the core principles in developing a virtual reality-based cognitive treatment, its strengths and weaknesses as a rehabilitation approaches
- Explain the use of a Budget application (APP) on an I-Pad and its potential use in cognitive rehabilitation
- Report advances in the assessment of cognition and everyday life in persons with TBI
Exoskeleton-Assisted Walking for Persons With Neurological Conditions, Part II: The State of the Art #1162
SAT // 12:30 PM – 2:00 PM
Faculty
Allan J. Kozlowski, PhD, BSc (PT), Icahn School of Medicine, Mount Sinai, New York, NY; Ann M. Spungen, EdD, VA RR&D National Center of Excellence for the Medical Consequences of Spinal Cord Injury, James J. Peters VA Medical Center, Bronx, NY; Candy Tefertiller, PT, DPT, ATP, NCS, Craig Hospital, Englewood CO; Gail F. Forrest, PhD, Rutgers, Newark, NJ; Clare Hartigan, PT, MPT, Crawford Research Institute, Shepherd Center, Atlanta, GA; Nicholas Evans, MHS, ACSM-CES, Shepherd Center, Atlanta, GA; Arun Jayaraman, PT, PhD, Max Nader Center for Rehabilitation Technologies & Outcomes Research, Rehabilitation Institute of Chicago Center for Bionic Medicine, Chicago, IL; Donald Peck Leslie, MD, Shepherd Center, Atlanta, GA; Chester Ho, MD, University of Calgary Foothills Hospital, Calgary, AB, Canada
Diagnosis/Area of Practice: Cross-Cutting
Focus: Technology (e.g., prosthetics/orthotics, robotics, assistive technology)
Powered exoskeletons offer persons with walking limitations due to neurological conditions opportunities to reengage in over-ground walking as a routine/therapeutic activity. Researchers are exploring the effects of exoskeleton-assisted walking for persons with spinal cord injury and other neurological conditions. However, we have limited evidence for the benefits and risks of short term use of this new technology, and know less about the long-term effects. Two moderators will lead a panel of clinical and research experts on the promise and the pitfalls of implementing powered exoskeleton technology into clinical practice and community use.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Describe characteristics of current clinical and wellness programs for conventional over-ground, bodyweight support treadmill, and powered exoskeleton-assisted walking for persons with neurological lower extremity paralysis or weakness
- Discuss three reasons that support implementation of available powered exoskeletons to rehabilitation and community wellness programs, and personal use; and the associated risks of doing so
- Discuss three reasons that support delayed implementation of exoskeletons to rehabilitation and community wellness programs, and personal use; and the associated risks of waiting for sufficient evidence to accumulate
Mediating Entities in the Knowledge Translation Cycle as Catalysts for Organizational Change #1290
SAT // 12:30 PM – 2:00 PM
Faculty
Allen W. Heinemann, PhD, Northwestern University Feinberg School of Medicine, Rehabilitation Institute of Chicago, Chicago, IL; Jason H. Raad, PhD, Rehabilitation Institute of Chicago, Chicago, IL; Susan Magasi, PhD, University of Illinois at Chicago, Chicago, IL
Diagnosis/Area of Practice: Cross-Cutting
Focus: Clinical practice (assessment, diagnosis, treatment, knowledge translation/EBP)
Several models of Knowledge Translation (KT) have been proposed; however, the effectiveness of these models in changing rehabilitation clinicians’ attitudes and behavior remains uncertain. This symposium describes the importance of catalysts in mediating organizational change. We illustrate how the Rehabilitation Measures Database serves as a catalyst to enhance rehabilitation clinicians’ understanding of outcome measures in clinical rehabilitation. Speakers will describe the utility of KT models and then propose an updated model based on the assumption that effective KT may be achieved when an external entity that neither creates knowledge nor provides direct services acts as an independent knowledge catalyst.
Learning Objectives
To support the attainment of knowledge, competence, and performance, the learner should be able to achieve the following objectives:
- Compare and contrast contextual and individual models of Knowledge Translation
- Apply theories of KT to organizational change initiatives in a healthcare setting
- Demonstrate the utility of KT catalysts in mediating organizational change
- Design organizational change initiatives using KT catalysts to promote evidence-based practice
Oral Presentation of Scientific Papers — Mild TBI/Cognitive Rehabilitation Topics
SAT // 12:30 PM – 1:30 PM
Moderator: Keith Cicerone, PhD, ABPP, FACRM
12:30 – 12:50: The Contribution of Psychological Factors to Recovery After Mild Traumatic Brain Injury: Prospective Cohort Study (#1511)
Presented by Deborah Snell
12:50 – 1:10: Headache Trajectory and the Development of Post Traumatic Stress Disorder After Mild Traumatic Brain Injury (#1639)
Presented by Jeanne Hoffman
1:10 – 1:30: The effect of two cognitive interventions on improving self-efficacy in persons with executive dysfunction post-stroke (#1537)
Presented by Valérie Poulin
ACRM Board of Governors Meeting (by invitation)
SAT // 2:30 PM – 6:30 PM
SUNDAY, 12 OCTOBER 2014
ACRM Board of Governors Meeting (by invitation)
Sun // 8:00 AM – 12:00 PM