Here at ACRM, we have a wide range of interdisciplinary interest groups, including one on neuroplasticity. In today’s blog post, we’re sharing a general overview on neuroplasticity, or the ability of neural networks in the brain to change or grow through reorganization. Neuroplasticity is an exciting field within rehabilitation medicine, and the findings of this type of rehabilitation research can help practitioners in many different areas, from TBI recovery to psychology and more. Continue reading to learn more, join the ACRM Neuroplasticity Networking Group, and register for this year’s conference!
What is Neuroplasticity?
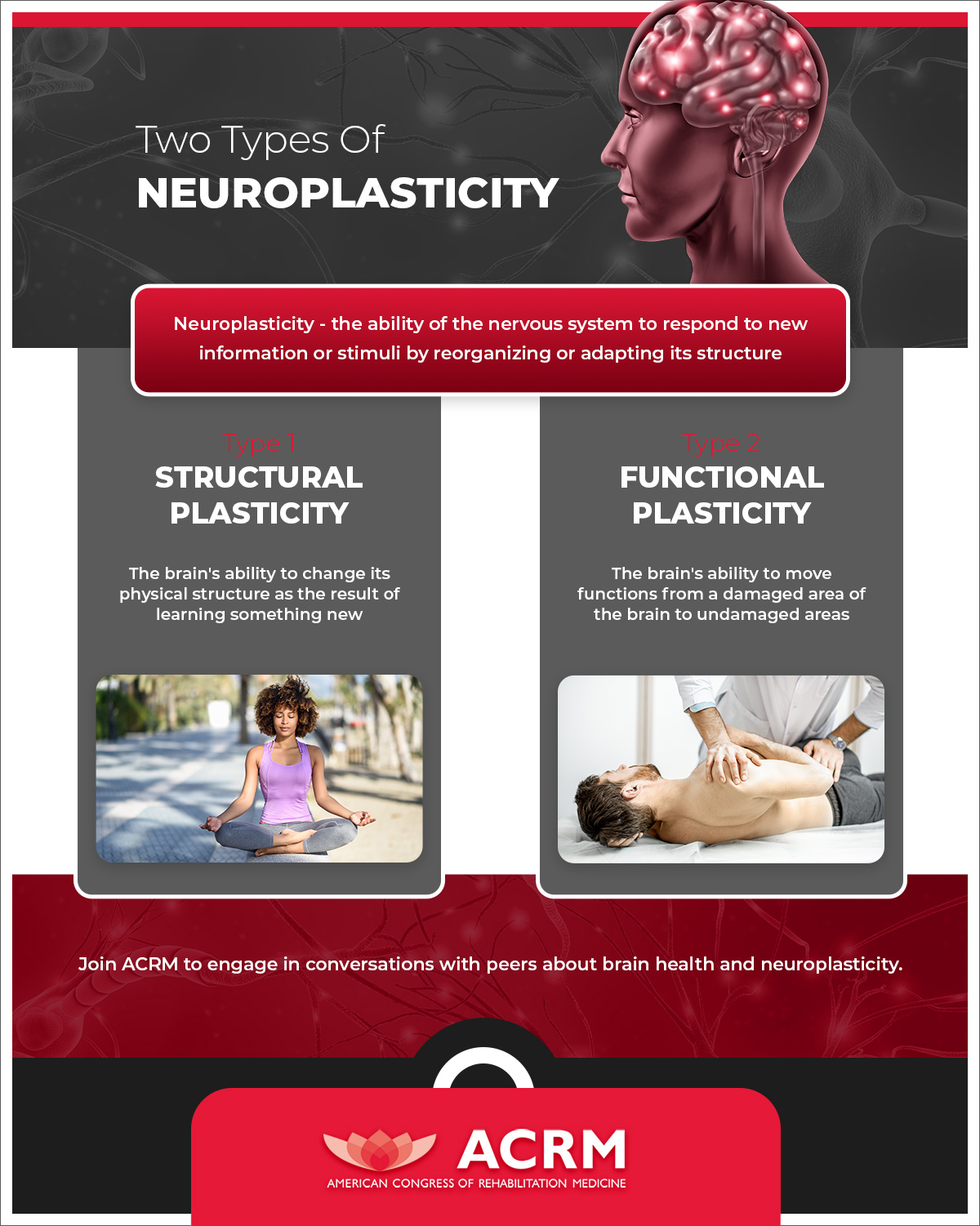
Neuroplasticity refers to the ability of the nervous system to respond to new information or stimuli by reorganizing or adapting its structure. This dynamic reorganization can play a role in rehabilitation from things like stroke, TBI, and even neurological diseases such as MS and Parkinson’s disease.
Neuroplasticity, or brain plasticity, is essentially the brain’s ability to change and adapt as a result of an experience. There are two main types of neuroplasticity:
Functional plasticity
Functional plasticity is the ability to move functions from a damaged area of the brain to undamaged areas. Functional plasticity changes occur in response to malfunction or damage of neurons and is a reactive type of neuroplasticity.
Structural plasticity
Structural plasticity is the ability to change the physical structure as the result of learning something new. New neurons are produced and integrated through the central nervous system as we learn and grow. The changes in the proportion of grey matter or synaptic strength are examples of structural plasticity. For example, a sustained meditation practice can lead to a higher proportion of grey matter in the brain.
Applications
There are many ways that neuroplasticity can, and is, being utilized in the field of rehabilitation medicine. Neuroplasticity demonstrates that the brain is not “hard-wired” with fixed circuits and that the brain can grow, change, and develop well into old age. Here are just a few, and if you join the ACRM Neuroplasticity Networking Group, you can dive further into the research and application.
Treatment of Brain Damage
With functional plasticity, as stated earlier, brain activity associated with a given function can be transferred from a damaged area of the brain to an undamaged area. Neuroplasticity explains, at least in part, the functional outcomes of physical therapy after a stroke, as patients improve function with an affected limb through therapies like constraint-induced movement therapy or functional electrical stimulation.
Meditation
Studies have linked meditative practices to the differences in thickness or density of gray matter. Meditation and mindfulness may be a way to utilize neuroplasticity to help treat anxiety, depression, fear, and anger by changing the physical structure of the brain.
Pain Management
Those who suffer from chronic pain may experience pain at sites that may have been previously injured but are now otherwise currently healthy. This chronic pain may be caused by a maladaptive reorganization of the nervous system. With advances in the understanding of neuroplasticity, practitioners may be able to reprogram the way the nervous system responds to signals and how the brain interprets this pain. Examples include using mirror therapy to treat phantom limb pain or meditation to help manage fibromyalgia. The goal of pain management therapy is to help reduce the overactive pain signals in the nervous system, and neuroplasticity may help in this.
Exercise
Aerobic exercise promotes adult neurogenesis, and consistent aerobic exercise can improve executive function and increase gray matter in multiple brain areas. Exercises increase the production of neurotrophic compounds, such as the brain-derived neurotrophic factor, BDNR, which can give rise to positive neuroplastic changes.
Deafness and Blindness
Those individuals with hearing loss have enhanced vision or other senses, as their auditory cortex is used to serve other functions than hearing. The same is true for individuals with vision loss, whose other senses may have enhanced abilities. For example, some blind people have developed human echolocation to navigate and sense their surroundings. Studies have shown that people who navigate with click-echos process those sounds in brain regions devoted to vision rather than hearing.
Multilingualism
Learning multiple languages can increase the brain’s capacity for plasticity. While more research needs to be done, studies have shown that bilinguals have longer attention spans, and strong organization and analysis skills.
ACRM – American Congress of Rehabilitation Medicine
The mission of our non-profit organization is to support the community of rehabilitative medicine professionals. We do so both in professional networking and our annual conference, and also through resources such as this blog. We work with hospitals, universities, professional, and advocacy organizations, and rehabilitation professionals around the world. We have 3,000+ members from more than 65 countries and proudly produce the ACRM Journal. Learn about the benefits of joining ACRM as well as membership dues and how to apply. You can also learn more about the ACRM Conference and register either in person or online here. We also offer ways to earn continuing education credits (CME/CEUS). Learn more here.