2021 Annual Conference Special Lecture Series
We have an exciting line-up for #ACRM2021 and our special lectures are no exception! Attendees have access to these recorded sessions with CME/CEUs through March 2022. Didn’t attend the Conference? No problem! Buy access now to the ACRM 2021 VIRTUAL Annual Conference with discount code: instantcme/ceus and save 15% on your purchase.
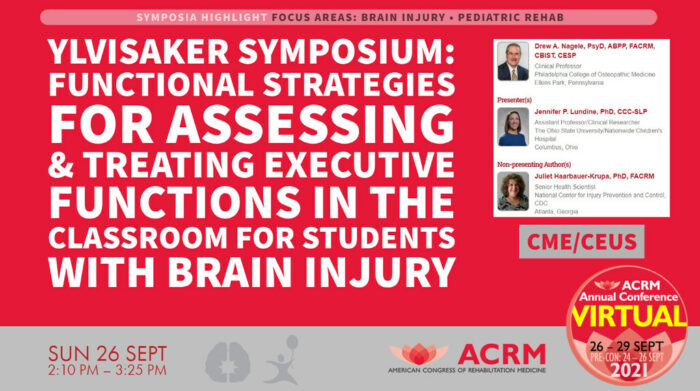
2021 Mark Ylvisaker Memorial Pediatric Brain Injury Symposium
Functional Strategies for Assessing & Treating Executive Functions in the Classroom for Students with Brain Injury
Speaker: Jennifer P. Lundine, PhD, CCC-SLP
Mark Ylvisaker believed that “in the absence of meaningful engagement in chosen life activities, all interventions will ultimately fail.” For children with acquired brain injury (ABI), the classroom provides the perfect setting to establish contextually meaningful interventions for cognitive and communication challenges. The subtle cognitive-communication and executive function difficulties experienced by students with ABI are often missed, leaving these students with unmet needs in the school environment and increasing the likelihood for negative social, academic, and vocational outcomes.
For children and adolescents with ABI, nonstandardized assessment offers several advantages over standardized assessment procedures, and may improve clinicians’ and educators’ abilities to identify students who might benefit from intervention services. This symposium discusses curriculum-based assessment and discourse analysis specifically, with additional focus on dynamic assessment procedures and task analysis.
Consistent with the philosophy of Mark Ylvisaker, nonstandardized assessment lends itself to the direct creation of intervention plans meant to target a student’s functional limitations as relevant to the classroom or school environment. Case studies will be used to demonstrate how these procedures can be implemented within the school environment to identify children who might benefit from supportive services. Nonstandardized assessment procedures are a valuable tool to measure a student’s cognitive-communication and executive function abilities and the effects of intervention in real-world contexts for students with ABI.
Access this symposium in the Online Program through March 2022 with your paid registration.
 Dr. Jennifer Lundine is an Assistant Professor in the Department of Speech and Hearing Science at The Ohio State University and is the director of the Childhood Cognition, Communication, and Brain Injury Lab (CABI Lab) Jenny completed both her BA in Speech and Hearing Science and MA in Speech-Language Pathology from The Ohio State University. She then worked as a speech-language pathologist on the rehabilitation unit and in acute care at Nationwide Children’s Hospital in Columbus for more than a decade before returning to OSU for her doctoral work.
Dr. Jennifer Lundine is an Assistant Professor in the Department of Speech and Hearing Science at The Ohio State University and is the director of the Childhood Cognition, Communication, and Brain Injury Lab (CABI Lab) Jenny completed both her BA in Speech and Hearing Science and MA in Speech-Language Pathology from The Ohio State University. She then worked as a speech-language pathologist on the rehabilitation unit and in acute care at Nationwide Children’s Hospital in Columbus for more than a decade before returning to OSU for her doctoral work.
She graduated with her PhD in Speech & Hearing Science in 2016, and continued her work at Nationwide Children’s Hospital as the Director of Research for the Department of Speech Pathology and the Inpatient Rehabilitation Program. She joined the faculty at OSU in the fall of 2017, and she remains an affiliated research scientist at Nationwide Children’s.
Dr. Lundine teaches courses in Cognitive-Communication Disorders, Pediatric Medical Speech-Language Pathology, and Language Acquisition. Her clinical, teaching, and research interests include impairments associated with complex pediatric medical diagnoses, especially cognitive-communication disorders associated with acquired brain injury (ABI). Specifically, her research focuses on improving gaps in access to and utilization of services designed to support children with ABI and identifying specific approaches that would improve assessment and treatment practices following pediatric ABI.
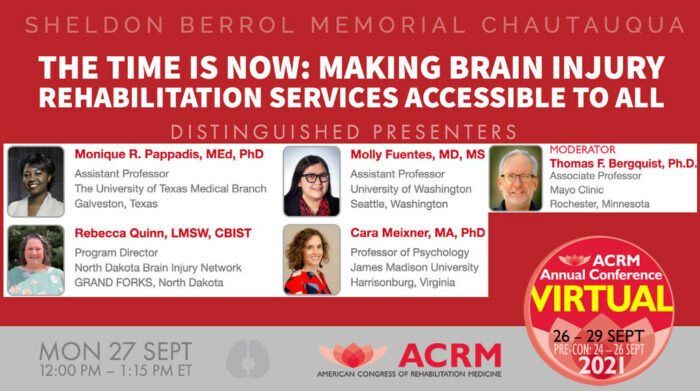
2021 Sheldon Berrol Chautauqua Symposium
The Time is Now: Making Brain Injury Rehabilitation Services Accessible to All
Access to rehabilitation services has become increasing difficult following traumatic brain injuries (TBI). Barriers not only include location of services and insurance funding but racial, ethic, and gender disparities. This symposium will present insights on barriers to service access, particularly for groups impacted by these barriers. Models and solutions to improve access to rehabilitation services for individuals who experience TBI will be discussed.
The Sheldon Berrol Chautauqua Symposium, named to honor Dr. Shelly Berrol’s famous “Let’s talk” invitation to his colleagues and friends, the Sheldon Berrol Chautauqua is the BI-ISIG special annual venue in which we address timely and sometimes controversial issues.
Access this symposium in the Online Program through March 2022 with your paid registration.
Moderator: Tom Bergquist, PhD, ABPP, Chair, BI-ISIG Executive Committee
 Thomas F. Bergquist, PhD, ABPP, FARCM, is an Associate Professor of Psychology in the Mayo Clinic College of Medicine and Co-investigator of the NIDILRR-funded Mayo TBI Model System Center. He is a member of the ACRM Board of Governors and chair of ACRM’s BI-ISIG. Dr. Bergquist has given numerous regional, national, and international presentations in the areas of brain injury rehabilitation and disability and has authored or co-authored over 35 journal publications in rehabilitation and medical journals.
Thomas F. Bergquist, PhD, ABPP, FARCM, is an Associate Professor of Psychology in the Mayo Clinic College of Medicine and Co-investigator of the NIDILRR-funded Mayo TBI Model System Center. He is a member of the ACRM Board of Governors and chair of ACRM’s BI-ISIG. Dr. Bergquist has given numerous regional, national, and international presentations in the areas of brain injury rehabilitation and disability and has authored or co-authored over 35 journal publications in rehabilitation and medical journals.
His principal research interests include rehabilitation following brain injury and coping with disability. He is a member of the board of directors of the Minnesota Brain Injury Alliance. He serves as a clinical supervisor at Compassion Counseling Center which provides mental health services to persons in SE Minnesota free of charge.
Disparities in Accessing Rehabilitation Services
Racial, ethnic and gender disparities can create barriers to accessing rehabilitation for persons with brain injury. This talk will describe these barriers and provide insights into care access.
 Monique R. Pappadis, MEd, PhD, is an Assistant Professor in the Division of Rehabilitation Sciences at the University of Texas Medical Branch at Galveston (UTMB) and an Investigator at the Brain Injury Research Center of TIRR Memorial Hermann. Her research aims to address improving rehabilitation outcomes and decreasing ethnic minority health disparities, particularly among persons with TBI or stroke. Her recent research focuses on care transitions and continuity of care following acute and post-acute care among older adults with TBI. She has a continued interest in minority aging, gender/sex disparities in rehabilitation, health literacy of patients and caregivers, and psychosocial adjustment to disability. She is a member of the ACBIS Board of Governors of the Brain Injury Association of America.
Monique R. Pappadis, MEd, PhD, is an Assistant Professor in the Division of Rehabilitation Sciences at the University of Texas Medical Branch at Galveston (UTMB) and an Investigator at the Brain Injury Research Center of TIRR Memorial Hermann. Her research aims to address improving rehabilitation outcomes and decreasing ethnic minority health disparities, particularly among persons with TBI or stroke. Her recent research focuses on care transitions and continuity of care following acute and post-acute care among older adults with TBI. She has a continued interest in minority aging, gender/sex disparities in rehabilitation, health literacy of patients and caregivers, and psychosocial adjustment to disability. She is a member of the ACBIS Board of Governors of the Brain Injury Association of America.
Barriers to Rehabilitation Care in Rural Communities
Living in rural communities often creates barriers to accessing rehabilitation. These barriers can include difficulties with copayments and lack of availability or transportation to a facility. This talk will describe the program implemented as part of the Brain Injury Network in the state of North Dakota. Barriers and issues observed with accessing rehabilitation will be discussed.
 Rebecca Quinn, LMSW, CBIST, is a program director for the Center for Rural Health at the University of North Dakota (UND) School of Medicine & Health Sciences in Grand Forks. Rebecca manages the North Dakota Brain Injury Network, and the State Epidemiological Outcomes Workgroup project. Rebecca’s past experience includes working in various settings, primarily in the healthcare field. She served as an adjunct professor in the Social Work department at UND where she taught courses on gerontology and substance abuse. Rebecca is a licensed social worker and obtained her master of social work degree from the University of Texas at Arlington in May 2000 and her bachelor of arts degree from Texas A & M in 1997.
Rebecca Quinn, LMSW, CBIST, is a program director for the Center for Rural Health at the University of North Dakota (UND) School of Medicine & Health Sciences in Grand Forks. Rebecca manages the North Dakota Brain Injury Network, and the State Epidemiological Outcomes Workgroup project. Rebecca’s past experience includes working in various settings, primarily in the healthcare field. She served as an adjunct professor in the Social Work department at UND where she taught courses on gerontology and substance abuse. Rebecca is a licensed social worker and obtained her master of social work degree from the University of Texas at Arlington in May 2000 and her bachelor of arts degree from Texas A & M in 1997.
Barriers and Facilitators of Rehabilitation Care among American Indian and Alaska Native People and Communities
Disparities in rehabilitation, including in access to services, for American Indian and Alaska Native people will be described. Barriers to rehabilitation care for AI/AN communities will be examined at multiple levels. Potential facilitators of rehabilitation for AI/AN individuals and communities will be shared.
 Dr. Molly Fuentes, MD, MS, is an Assistant Professor of Rehabilitation Medicine at the University of Washington School of Medicine with a clinical practice in Pediatric Rehabilitation Medicine at Seattle Children’s Hospital. She attended the University of Michigan Medical School (MD ’08) and completed residency in Physical Medicine and Rehabilitation at the University of Washington, also serving as Chief Resident. Dr. Fuentes then completed a clinical fellowship in Pediatric Rehabilitation Medicine at Seattle Children’s and then a research fellowship at the Harborview Injury Prevention and Research Center and an MS in Health Services from the UW School of Public Health before joining the faculty of UW. Her research focuses on inequities in rehabilitation and functional outcomes for American Indian and Alaska Native children with disabilities as well as access to rehabilitation services. Dr. Fuentes is a citizen of the Confederated Tribes of Warm Springs and grew up in Warm Springs, Oregon.
Dr. Molly Fuentes, MD, MS, is an Assistant Professor of Rehabilitation Medicine at the University of Washington School of Medicine with a clinical practice in Pediatric Rehabilitation Medicine at Seattle Children’s Hospital. She attended the University of Michigan Medical School (MD ’08) and completed residency in Physical Medicine and Rehabilitation at the University of Washington, also serving as Chief Resident. Dr. Fuentes then completed a clinical fellowship in Pediatric Rehabilitation Medicine at Seattle Children’s and then a research fellowship at the Harborview Injury Prevention and Research Center and an MS in Health Services from the UW School of Public Health before joining the faculty of UW. Her research focuses on inequities in rehabilitation and functional outcomes for American Indian and Alaska Native children with disabilities as well as access to rehabilitation services. Dr. Fuentes is a citizen of the Confederated Tribes of Warm Springs and grew up in Warm Springs, Oregon.
An Ethical Framework to Promote Health Systems Change for Access to Rehabilitation
Brain Injury survivors with long-term needs often encounter precarious situations where they struggle to receive services in health systems focused on cost containment driven by medical necessity and managed care. This talk will describe a framework for consideration to help improve access to care.
 Cara Meixner, PhD, is Professor of Graduate Psychology at James Madison University, where she teaches graduate courses in research methodology and serves as methodologist on various theses and dissertations. Dr. Meixner is a scholar of research methods with keen interest in epistemology, ontology, and the philosophy of science. Related to neurotrauma, she pursues an advocacy-based research agenda that has contributed to the development of noteworthy changes and advocacy initiatives for survivors of brain injury. She has served as co-principal investigator, with Dr. Cynthia O’Donoghue, on studies that investigate barriers to accessing crisis intervention services, with focus on the experience of survivors with neurobehavioral presentations. More recent research focuses on the caregiver-survivor experience and the intersection between neuroethics and access to care. Publication venues include Brain Injury, Journal of Head Trauma Rehabilitation, and NeuroRehabilitation. Dr. Meixner currently serves as a state-level appointee to the Virginia Brain Injury Council, where she was recently elected chairperson.
Cara Meixner, PhD, is Professor of Graduate Psychology at James Madison University, where she teaches graduate courses in research methodology and serves as methodologist on various theses and dissertations. Dr. Meixner is a scholar of research methods with keen interest in epistemology, ontology, and the philosophy of science. Related to neurotrauma, she pursues an advocacy-based research agenda that has contributed to the development of noteworthy changes and advocacy initiatives for survivors of brain injury. She has served as co-principal investigator, with Dr. Cynthia O’Donoghue, on studies that investigate barriers to accessing crisis intervention services, with focus on the experience of survivors with neurobehavioral presentations. More recent research focuses on the caregiver-survivor experience and the intersection between neuroethics and access to care. Publication venues include Brain Injury, Journal of Head Trauma Rehabilitation, and NeuroRehabilitation. Dr. Meixner currently serves as a state-level appointee to the Virginia Brain Injury Council, where she was recently elected chairperson.
2021 Joshua B. Cantor Scholar
The Cantor Scholar Award is presented by the Brain Injury Interdisciplinary Special Interest Group (BI-ISIG) to a BI-ISIG member in recognition of outstanding research that is judged to be a significant contribution to the field of brain injury rehabilitation.
The award is named in honor of Dr. Joshua B. Cantor, who was renowned for his research on the effects of cognitive fatigue, sleep deprivation, and exercise on various aspects of life after TBI. His work also included efforts to enhance cognition and reduce depression, primarily through problem-solving and emotion regulation training interventions. Dr. Cantor’s work was driven by his passion for developing and evaluating interventions that would give solace, meaning, and hope to individuals with TBI.

Dr. Shannon Juengst is an Assistant Professor in the Department of Physical Medicine & Rehabilitation at the University of Texas Southwestern Medical Center. She also holds a secondary appointment in the Department of Applied Clinical Research. She is a certified rehabilitation counselor. Dr. Juengst leads a compelling program of research focusing on improving the lives of individuals with injury to the central nervous system and their caregivers. Her primary research focus is on individuals with Traumatic Brain Injury (TBI). Her secondary research foci include individuals with stroke and individuals with other acquired and neurodegenerative conditions. The major areas of her research comprise developing efficient methods for long-term monitoring of individuals with cognitive, emotional, and behavioral sequelae and implementing targeted interventions to improve these sequelae. In her work, she also uses smartphone and other mobile applications to improve health outcomes. Her research also aims to minimize health disparities by translating work in Spanish and culturally adapting for Spanish-speaking people throughout her research.
Dr. Juengst’s research is supported by major funding agencies such as the National Institute of Health, the National Institute for Disability, Independent Living, and Rehabilitation Research (NIDILRR), and Texas Alzheimer’s Research & Care Consortium (TARCC). She has also received funding from numerous professional foundations. Dr. Juengst has published over 70 referred papers, including about 28 first-author peer-reviewed papers. She has taught over 15 courses, including courses in rehabilitation counseling, neurorehabilitation theory and practice, evidence-based practice, and practical issues in disability. She has also mentored over 30 undergraduate, graduate, and doctoral trainees. Her excellence in research and teaching is recognized by numerous research and teaching awards that she has received over the years. Dr. Juengst is an active leader within ACRM.
2021 Edward Lowman Award

ACRM is pleased to honor Kristen Dams-O’Connor, PhD, FACRM, with the 2021 Edward Lowman Award. The Award was established in 1989 in honor of Edward Lowman, MD, and recognizes ACRM members whose careers reflect an energetic promotion of the spirit of interdisciplinary rehabilitation. Dr. Dams-O’Connor is Director of the Brain Injury Research Center of Mount Sinai and Professor in the Departments of Rehabilitation Medicine and Neurology at Icahn School of Medicine at Mount Sinai. This award will be presented during the ACRM 2021 VIRTUAL Annual Conference.
Kristen Dams-O’Connor, PhD, FACRM, is Director of the Brain Injury Research Center of Mount Sinai and Professor in the Departments of Rehabilitation Medicine and Neurology at Icahn School of Medicine at Mount Sinai in New York, NY. She conducts multidisciplinary research dedicated to improving the lives of people living with brain injury. Her work aims to identify mechanisms, risk and protective factors to improve long-term outcomes in individuals with traumatic brain injury (TBI) and repetitive head trauma sustained through sports participation, military service, and intimate partner violence.
Her team uses modern psychometric and statistical techniques to measure individual differences in trajectories of change over time among survivors of TBI. One goal of this work is to improve diagnosis of secondary post-traumatic conditions during life so they can be treated. She leads the Late Effects of TBI (LETBI) Project, a TBI brain donor program focused on characterizing the clinical phenotype and postmortem pathological signatures of post-traumatic neurodegeneration and their associations with Alzheimer’s disease and related dementias.
Dr. Dams-O’Connor is Project Director of the New York Traumatic Brain Injury Model System of care, one of 16 centers of excellence for TBI research and clinical care in the United States. Her research is supported by federal grants from the National Institutes of Health, National Institute for Disability Independent Living and Rehabilitation Research, Department of Defense, Centers for Disease Control, and Patient Reported Outcomes Research Institute. She has published over 100 peer-reviewed manuscripts and chapters on TBI treatments and outcomes, and has presented her research internationally.
BI-ISIG MEMBERS HONORED WITH 2021 BIAA AWARDS
2021 Trexler Dissertation Award
The Role of FK506-binding Protein 51 (FKBP5) in Long-term Psychosocial Outcomes of Pediatric TBI
Dissertation Grant of $5,000 supported by Dr. Lance and Laura Trexler
Grantee: Dana Lengel, Drexel University
Mentor: Ramesh Raghupathi, PhD
Childhood Traumatic Brain Injury (TBI) results in increased risk for psychosocial disorders that can emerge in adolescence and adulthood. This vulnerability may be due to the susceptibility of developing neural stress circuits to TBI. In this proposal, we investigate the role of FK506-binding protein 51 (FKBP5), a co-chaperone of the glucocorticoid receptor (GR) and psychiatric risk factor, in behavioral and neuroendocrine effects of social stress following pediatric TBI. Targeting the GR system through FKBP5 may be able to mitigate the risk for psychosocial disorders following childhood TBI.
 Dana Lengel is a fifth-year PhD student in the Raghupathi Lab. She is originally from Long island, New York. She received her bachelor’s degree in psychology from Queens College and then completed a master’s degree in neuroscience from Stony Brook University. Her overall research interests include brain injury, stress, early life adversity and sex differences. Her dissertation project is focused on investigating the role of glucocorticoid receptor dysfunction within the hippocampus on vulnerability to stress and cognitive deficits following pediatric traumatic brain injury.
Dana Lengel is a fifth-year PhD student in the Raghupathi Lab. She is originally from Long island, New York. She received her bachelor’s degree in psychology from Queens College and then completed a master’s degree in neuroscience from Stony Brook University. Her overall research interests include brain injury, stress, early life adversity and sex differences. Her dissertation project is focused on investigating the role of glucocorticoid receptor dysfunction within the hippocampus on vulnerability to stress and cognitive deficits following pediatric traumatic brain injury.
 Dr. Raghupathi is a professor in the Department of Neurobiology & Anatomy at Drexel University College of Medicine. He did postdoctoral training at the University of Connecticut Health Science Center and the University of Pennsylvania School of Medicine. Before coming to the College of Medicine in 2003, he served on the faculty in the Department of Neurosurgery at the University of Pennsylvania School of Medicine.
Dr. Raghupathi is a professor in the Department of Neurobiology & Anatomy at Drexel University College of Medicine. He did postdoctoral training at the University of Connecticut Health Science Center and the University of Pennsylvania School of Medicine. Before coming to the College of Medicine in 2003, he served on the faculty in the Department of Neurosurgery at the University of Pennsylvania School of Medicine.