COVID-19 Q&A with Incoming BI-ISIG Executive Committee Members

Angelle Sander, PhD, FACRM
Angelle M. Sander, PhD, FACRM
2020-2022 BI-ISIG Chair-Elect
Neuropsychologist
Baylor College of Medicine and TIRR Memorial Hermann
Houston, TX- inpatient and outpatient rehabilitation and research
Angelle M. Sander, PhD is Associate Professor with tenure in the Department of Physical Medicine and Rehabilitation at Baylor College of Medicine and is Director of the Division of Clinical Neuropsychology and Rehabilitation Psychology. She is also Director of TIRR Memorial Hermann’s Brain Injury Research Center and Senior Scientist on the TIRR Research Council. She has been PI or Co-Investigator on over 20 federally funded studies addressing prediction and treatment of cognitive, emotional, and psychosocial problems in persons with TBI, intimacy and sexuality after TBI, impact of TBI on caregivers, and cultural disparities in outcomes following TBI. She co-chairs the TBI Model System Special Interest Group on Caregivers and Families, as well as the Cultural Competency Special Interest Group. She has over 100 peer-reviewed publications, numerous book chapters and published abstracts, and multiple consumer-oriented dissemination products, including fact sheets, educational manuals, webcasts, and videos. Dr. Sander also serves as neuropsychologist for the inpatient rehabilitation unit at CHI Baylor St. Luke’s Medical Center.
Q: What are you doing to care for yourself and reduce professional burnout during the COVID-19 pandemic?
A: Gratitude has helped me immensely in coping with the pandemic. I am taking time to notice things that I am grateful for daily- a momentary cool breeze early in the morning when I let my dogs outside, or a particularly good iced coffee, and always my family. I am trying to approach everything in a mindful way- noticing little things and realizing how lucky I am. Spending extra time with my immediate family, without the hustle and bustle of our pre-COVID lives, has been a blessing. After a full day of Zoom meetings and online work, it is wonderful not to have to sit in traffic coming home- but just transition to a new ritual of ending the work day by joining my daughter to watch an episode or two of our favorite shows (Gilmore Girls, Glee, or Grey’s Anatomy).
Q: Has your location been overwhelmed and have you experienced PPE shortages? How has this been addressed?
A: At Baylor College of Medicine and at TIRR Memorial Hermann, we have been lucky to continue seeing rehabilitation patients in the usual way, and to not have our inpatient units transitioned to COVID care facilities. This is likely because of the amazing number and quality of acute hospitals in the Houston area. We also benefitted from learning from cities like New York, that experienced a COVID surge early during the pandemic. Our surge occurred later, and we had time to prepare by stockpiling PPE and planning for staff and space needs. We did not experience a PPE shortage because of this, and this helped to keep our staff morale high.
Q: How has your job (and/or life) changed due to the pandemic?
A: Work is different due to having our research assistants and other staff working from home and not being able to meet in-person; however, we have a great team who has been able to maintain productivity and quality during the pandemic. We meet regularly via Zoom and phone calls, and I honestly have not perceived a change in what we are able to accomplish. What I miss most is being able to meet with friends and colleagues in person. The Zoom meetings are great, but they are not the same. Missing in-person meetings, like ACRM, where we can have informal conversations over dinner and drinks, is a loss. And not being able to visit family in other states is painful. I look forward to in-person happy hours, meetings, and hugs when this is over!
Q: What gives you hope related to the pandemic?
A: I know that we have the best of medical minds working to develop a safe and effective vaccine, and I am confident that they will accomplish this goal in the not-so-distant future. Knowing that this situation is temporary allows me to have hope. Also, we have learned a lot from the pandemic that we can use to prepare for future pandemics. I also happen to live in a city (Houston) with one of the best medical centers in the world, and I am confident that they are well prepared to care for anyone that becomes ill from COVID-19.
Q: Do you have any final thoughts regarding the pandemic you would like to share?
A: What the pandemic has taught me is that we are all in this together (not just the pandemic, but life). We must all be willing to sacrifice for the good of all, and we must be grateful for each day and show kindness to others. This is the only way that we can survive the pandemic and survive as a human race. The pandemic has brought out the best and the worst and people, but there has been much good, and that is what we need to focus on.
 Amanda Robinowitz, PhD
Amanda Robinowitz, PhD
2020-2022 BI-ISIG Secretary
Institute Scientist
Moss Rehabilitation Research Institute (MRRI)
Philadelphia, PA
Dr. Rabinowitz is a clinical neuropsychologist by training. She directs the Brain Injury Neuropsychology Laboratory, which conducts research on the cognitive and emotional consequences of TBI across levels of severity.
Q: What are you doing to care for yourself and reduce professional burnout during the COVID-19 pandemic?
A: Adjusting to the changes to work and home life related to the pandemic has certainly been a source of stress! Attending to self-care has been more important than ever for me to maintain my sanity and productivity during this time. Spending some time converting a guest room into a cozy and pleasant home office was a big help. I’ve also started a regular home workout routine. And I’ll admit, I’ve become one of those sourdough baking people!
Q: How has your job (and/or life) changed due to the pandemic?
A: Work at the research institute went fully remote when the pandemic reached its peak for our region of the country in March. For my lab, this meant changes to our day-to-day routine, as well as the suspension of research studies that required in-person contact. Fortunately, there was a good portion of our work that we could continue remotely—studies that mostly rely on telephone contact.
We also began adapting in-person study protocols so that they could be carried out remotely. This has presented a considerable challenge, as well as an opportunity to explore new methods of collecting data and delivering interventions. In order to maintain team contact and keep up moral among the lab, we have started to rely more heavily on software platforms for collaboration and team communication.
The pandemic has also brought major changes to home life. I have two sons, ages 3 and 5, who were suddenly home all day while my husband and I both attempted to keep up with our full-time jobs at home. This Fall my oldest son begins virtual Kindergarten from home, while my youngest son will be able to attend in-person preschool.
Q: As we move from an acute phase to a more chronic phase of the pandemic, has anything changed?
A: As we’ve moved to the chronic phase of the pandemic, we are starting to explore ways of returning to our usual activities safely and cautiously. A Re-opening Task Force at our Institute is currently developing guidelines and protocols for resuming in-person research. As COVID cases are declining in our region, the census on our inpatient unit has returned to normal, and our colleagues in the clinic have resumed some of their outpatient services. While all this is encouraging, it is also clear that without the necessary precautions, things could quickly change. Hence, as we cautiously look to resume our research, we’ve been rethinking our procedures and research methods to reduce reliance on in-person contact.
Q: Do you have any final thoughts regarding the pandemic you would like to share?
A: The pandemic has brought with it many challenges and hardships. It has also revealed opportunities for the PM&R field to reimagine how we provide rehabilitative care. A primary interest of mine is chronic TBI. Under usual circumstances, transportation and financial limitations are barriers to accessing care for this population. As clinicians and researchers have adapted to the circumstances of the pandemic, we’ve had to jump into the world of telemedicine and mobile health with both feet. Continued research and refinement of these remote-treatment-delivery methods could only improve access to care moving forward.
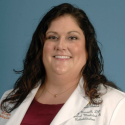 Mary E. Russell, DO, MS
Mary E. Russell, DO, MS
2020-2022 BI-ISIG Communications Officer
Assistant Professor and Vice Chair, Quality and Compliance
McGovern Medical School, University of Texas Health Science Center
TIRR Memorial Hermann – The Woodlands – inpatient and outpatient rehabilitation
Houston, TX
Mary E. Russell DO, MS, an Assistant Professor and Vice-Chair of Quality and Compliance in the Department of Physical Medicine and Rehabilitation at McGovern Medical School at UTHealth, completed her residency at the Baylor/University of Texas Physical Medicine & Rehabilitation Alliance in July 2014. She received her medical degree in 2010 from Des Moines University. She received her master’s degree in Biomedical Engineering from the University of Iowa in 2005, with an emphasis on musculoskeletal biomechanics. Dr. Russell cares for inpatient and outpatient patients recovering from stroke, traumatic brain injury, and neurotrauma. Her hospital affiliations include TIRR Memorial Hermann and Memorial Hermann Hospital-The Woodlands. She is an active member of the American Academy of Physical Medicine and Rehabilitation, the Association of Academic Physiatrists and American Congress of Rehabilitation Medicine. Dr. Russell also serves as the Medical Director at TIRR Memorial Hermann-The Woodlands. Her clinical interests include spasticity management and brain injury medicine. She is board certified in Physical Medicine and Rehabilitation and Brain Injury Medicine.
Q: What are you doing to care for yourself and reduce professional burnout during the COVID-19 pandemic?
A: In the past 18 months, I have gotten into playing pickleball and have found that it is a great activity for social connections, physical activity and to take my mind off work.
Q: Has your location been overwhelmed and have you experienced PPE shortages? How has this been addressed?
A: During our recent surge, we have been fortunate to have no issues within the system with bed capacity and PPE. The system is using CDC recommended guidelines and re-sterilizing N95s.
Q: How has your job (and/or life) changed due to the pandemic?
A: It definitely has reduced my personal bubble to 6 ft. and now is common to wear masks and goggles at work. Go out to eat less and have not been traveling.
Q: What gives you hope related to the pandemic?
A: I am hopeful that medical system changes may persist and expand, such as telemedicine, to offer persons with disabilities access to more resources.
Q: Do you have any final thoughts regarding the pandemic you would like to share?
A: It is an interesting time to be practicing medicine. As there have been other pandemics, it will be interesting to see what changes persist after this passes and what we learn.