Top Symposia Recommended for Stroke
These educational presentations are recommended by the Stroke ISIG as the top symposia for stroke presented at the ACRM 2020 VIRTUAL Annual Conference. Use your 2020 Conference registration to access these presentations virtually and earn CME/CEUs through June 2021. Not yet registered?
Rebuilding Identity and Rewarding Lives After Stroke: The Emotional Journey in Recovery (821008)
Presenters: Debra E. Meyerson, PhD, Steven A. Zuckerman, MBA, Kara Flavin, MD, Julie Muccini, MS, OTR/L, Leora R. Cherney, PhD, CCC-SLPHow do stroke survivors recover? Unless they return to exactly the life they enjoyed before the stroke, a critical component of recovery must include helping survivors on their emotional journey to redefine the self. This presentation will be led by Dr. Debra Meyerson, formerly a tenured professor at the Stanford School of Education who suffered a severe stroke in 2010. She and her husband share their experiences with the recovery process, and the work they are doing to better understand and support stroke survivors and families in rebuilding identity as a critical step toward rebuilding rewarding lives. Three professional care providers — a physiatrist, a speech-language pathologist and aphasia expert, and an occupational therapist — will talk about their experience in the rehabilitative process, how they support this aspect of recovery, and the research, resources, and practices they think could help the field of stroke recovery do so more effectively.
Combating Executive Functioning Deficits Through the Use of Smart Systems and Integrative Technologies
Presenters: Fofi Constantinidou, PhD, CCC-SLP, Eva Pettemeridou, PhD, Peter Meulenbroek, PhD, Tracey Wallace, CCC-SLP
This symposium addresses a significant challenge in TBI, namely the chronic deficits in executive functioning and self-awareness. These deficits often interfere with successful reintegration of TBI survivors in their educational and work settings. We will provide evidence from the use of smart multimodal intelligent systems (iPams) in identifying and monitoring emotional states. We will also present efficacy data on computer-assisted interventions targeting social communication training and return to work (WoRC training). These methods offer a safe environment in which to explore social skill strategies without consequences. We will conclude with the presentation of SwapMyMood, a smartphone application designed to optimize delivery and monitoring of metacognitive strategies in rehabilitation. The ultimate objective of these novel methodologies is to shift the burden of responsibility to the patient, minimize errors and maximize self-awareness and strategy use that can lead to effective performance
Epidemiology, Challenges, and Rehabilitation of Young Strokes
Presenters: Abiodun E. Akinwuntan, PhD, MPH, MBA; Samir R. Belagaje, MD; Suzanne Perea Burns, PhD, OTR; Megan Danzl, PT, DPT, PhD, NCS; Catherine C. Hay, PhD, OTR; Valerie Hill, PhD, OTR/L; Alexandra L. Terrill, PhD
This symposium will provide an overview on the topic of stroke in young adults. Specifically, the presenters will provide a summary of the epidemiology, review the challenges inherent to rehabilitation of this population and focus on the WHO’s 2019 seven dimensions of adult rehabilitation: Cognition, Mobility, Self-Care, Vision, Communication, Prevention, and Relationships.
College After Concussion: Care Across the Recovery Continuum (821912)
Presenters: Katy H. O’Brien, PhD, CCC-SLP, Tracey Wallace, CCC-SLP, Penny L. Welch-West, MClSc, SLP (C)
College students with concussion are a unique population because they are often away from home and their healthcare providers, unsure how to manage their healthcare needs, and have overall poor health and sleep hygiene. This presentation compares and contrasts two programs of care for college students with concussion, addressing needs from acute injury and peer support to reduce complicated recovery, through direct group intervention in a simulated classroom setting for students with persisting symptoms. Outcomes and student perspectives on the role of these programs in return to postsecondary education will be discussed as well.
End of Life Supportive Care in Neuro-oncology: The Role of Cognitive Rehabilitation (848211)
Presenters: Amy Maguire, MS, CCC-SLP, Byram Ozer, MD, PhD, Amy Maguire, MS, CCC-SLP
A critical aspect of cognitive rehabilitation in neuro-oncology is the higher likelihood that providers may need to incorporate end of life care. Cognitive rehabilitation specialists can play an important role in sustaining and improving quality of life and functioning during this critical period in patients’ lives. Delivering effective support can be simultaneously essential and quite challenging, however, including: cognitive and communication impairment, behavioral changes, environmental and mobility limitations, and the fundamental question of when and how to present such care. This symposium will highlight evidence-based intervention approaches, resources, and case examples across the lifespan, including pediatrics. The overall goal of this symposium is to outline the supportive role cognitive rehabilitation professionals can play during this sensitive phase, against the backdrop of shifting from a “recovery” mindset to one that focuses on maximizing quality of life and the patient’s personal sense of meaning.
Team Approaches to Addressing Dysphagia in a Patient with Food Aversion
Presenters: Renee Madathil, Rehab. Neuropsychologist; Sophie Wereley, SLP
Research Objectives: To examine the utility and feasibility of concurrent psychological interventions in treatment of dysphagia for an adult inpatient with food aversion. Design: Case study over the course of a 39 day inpatient stay. Setting: Acute inpatient rehabilitation unit in an academic medical center. Participants: This study follows the course of an adult patient who was identified to have both dysphagia and food aversion.
From Disability to Productivity: Transitioning to Employment, Volunteerism, and Caregiving Following Stroke (848392)
Presenters: Phillip Rumrill, PhD, CRC, Christina Dillahunt-Aspillaga, PhD. CRC, CVE, CLCP, CBIST
This symposium presents a definition of returning to productive activity (employment, volunteering, informal caregiving) after stroke combined with discussion about the value of resuming these activities for the person, third-party-payers, and society. We will discuss the analysis process of determining eligibility for work resumption, identifying community- and employer supports, and therapeutic strategies to facilitate a successful transition to the workforce. We will close with a discussion and reflection about evidence supporting the intervention process and gaps in existing literature.
Multidisciplinary Management of Sialorrhea in the Pediatric Population: Evidenced Based Practice and Clinical Outcomes (857487)
Presenters: Didem Inanoglu, MD, FAAPMR; Ashley Brown, MS, CCC-SLP, BCS-S; Allison Brown, MS, CCC-SLP, BCS-S
With advancements in medical care and technology, there is a rapidly growing group of children with complex medical conditions who have a significant secretion control problem. This session will discuss an interdisciplinary model of evidenced-based medical and therapeutic management of the patient with decreased secretion control. Discussion will include a review of current gap in knowledge and practice, the critical roles of key players within the interdisciplinary model, and current evidence informing clinical decision making. The knowledge base gained will enable providers to collaborate with various specialists to coordinate a cohesive and state of the art plan for their patients. The presenters will highlight techniques for saliva control within these patient populations from the perspectives of speech-language pathologists and physiatrists. The session will conclude with presentations of case studies and outcomes from our interdisciplinary program to provide guidance for program development and direction for future research for this critical population.
Evidence for Active Training Programs, Education, and Multidisciplinary Care Following Concussion (845879)
Presenters: Brian M. Moore, PT, DPT; Elisabeth (Lisa) C. D’Angelo, PhD, CCC-SLP
This session is designed for rehabilitation specialists who provide services to children, young adults, and older adults following a concussion, with an emphasis on sports-related concussion (SRC) as this is the most well-developed area described in the literature related to concussion. The purpose of this educational seminar is to provide a review of the evidence for active training and educational programs for children and adults with acute concussion and persistent post-concussion symptoms (PPCS). In addition, a special focus on the use of multidisciplinary treatment approaches used to address impairments for individuals with PPCS will be provided.
Music as an Effective Treatment for Challenging Cognitive and Motor Impairments: An Interprofessional Approach (849072)
Presenters: Leanna W. Katz, MS, OTD, OTR/L; Abigail Spaulding, PT, DPT, NCS; Caitlin R. Hyatt, MT-BC, Neurologic Music Therapist Fellow
Music can both facilitate and support therapeutic interventions for neurological impairment because of its unique ability to be measured and adapted to align with corresponding movement, cognition, and visual/perception. Recent literature demonstrates multiple theories on music processing and the use of music to promote brain plasticity in neurorehabilitation (Strait et al., 2009; Thaut & Hoemberg, 2014). This presentation will transform these theories into clinical implementation and provide the participants a toolset to utilize in practice.
Clinical Research Methodology: Lessons Learned from Experts in the Field of Aphasia (825397)
Presenters: Leora Cherney, PhD, CCC-SLP, Anastasia Raymer, PhD, Jaime Lee, PhD, CCC-SLP
Rehabilitation research encompasses many different research methods. This session provides foundational information about the design and conduct of methodologies that can be rigorously applied to answer clinical research questions. These include systematic reviews, single-case experimental studies, and clinical trials. Using examples primarily from their own work, three experts from the field of aphasia discuss lessons they learned while using these approaches. They offer some tips that they have discovered along the way as well as discuss pitfalls to avoid. Their examples will be supplemented with other recent compelling clinical studies in the area of aphasia research. Although this symposium offers examples from aphasia research, the information will be relevant to rehabilitation research in general.
Showing You Care About Stroke Through Shared Measures: How to Improve Clinical and Research Outcomes by Implementing Core Outcomes Measure Sets and Common Data Elements (841232)
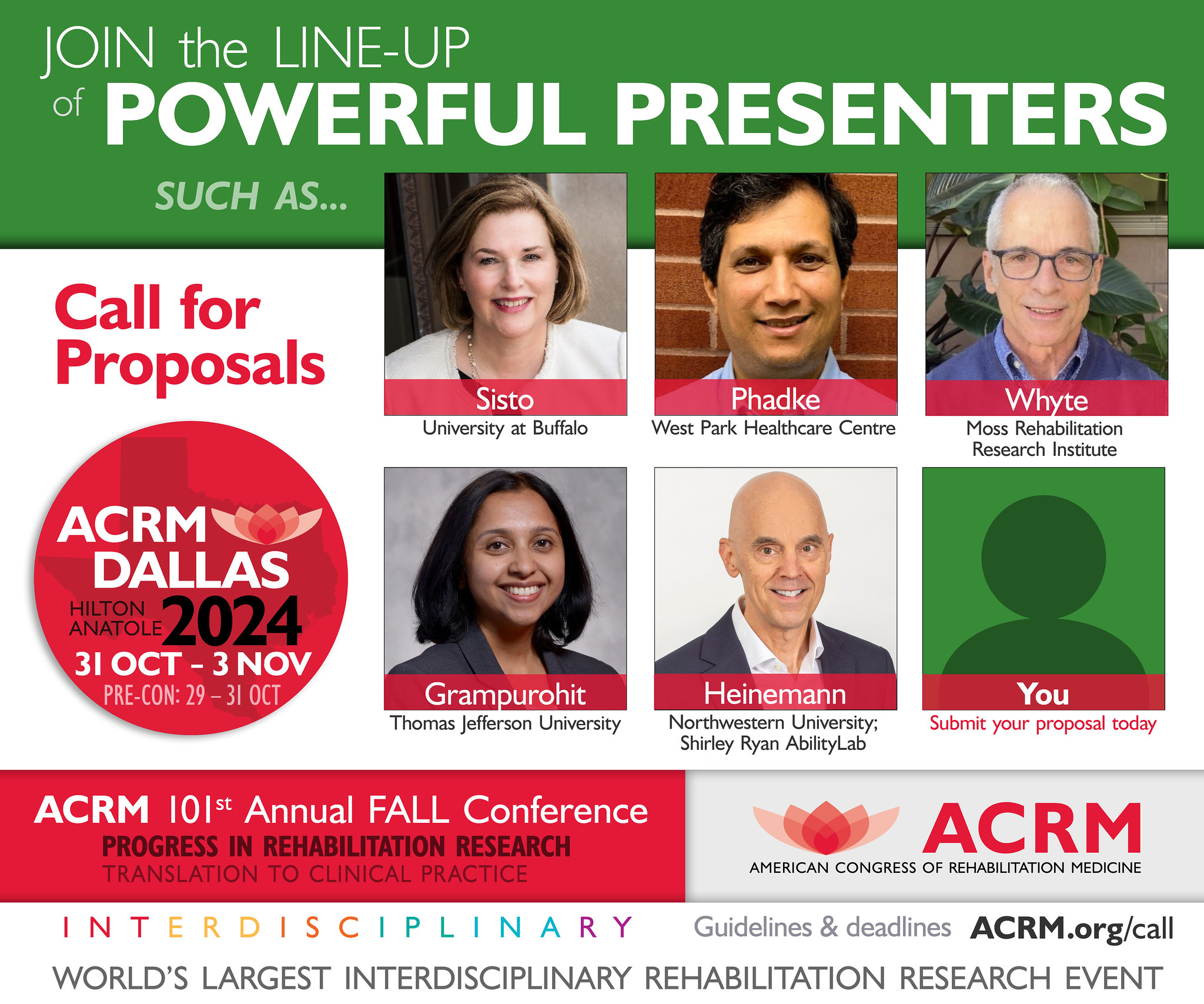
Presenters: Julie L. Schwertfeger, PhD; Lyn Jakeman, PhD; Susan H. Lin, ScD, OTR/L, FAOTA; Jennifer Weaver, MA, OTR/L, CBIS; Allen W. Heinemann, PhD, ABPP, FACRM photo; Stephanie A. Kolakowsky-Hayner, PhD, CBIST, FACRM ; William v. Padula, OD SFNAP FAAO FNORA ; Sarah J. Wallace, PhD BSpPath(Hons) Grad Cert in Geriatrics; Leora R. Cherney, PhD, CCC-SLP, BC-ANCDS, FACRM; Namrata Grampurohit, PhD, OTR/L; Julie Bernhardt, PhD
Stroke is the second leading cause of death and a major cause of disability worldwide. There are over 6.5 million people in the world living with the effects of stroke, and this number is expected to triple between 2010 and 2050 resulting in pressing issues for healthcare delivery, resources, and logistics that include annual care costs of $34 in the US alone. Core outcome sets (COS) and Common data elements (CDE) are designed to help clinicians, health systems, and researchers improve knowledge sharing, collaboration, and client outcomes. This symposium provides an overview of stroke COS and CDE. A clinical case highlights how the COS and CDE can improve outcomes, efficiencies, and data sharing. Initiatives and resources on developing and translating COS and CDE into practice and research will be explained. Clinical team and health outcome benefits will be illustrated. Audience discussion on barriers and facilitators will be included.
Clinical Applications of Longitudinal Mixed Effects Models (838334)
Presenters: Allan J. Kozlowski, PhD; Lynne Gauthier, PhD; Julie L. Schwertfeger, PhD
Many important rehabilitation outcomes evolve over weeks or even years after injury, yet common outcome assessment methods examine point-in-time events, such as at rehabilitation discharge. Researchers have begun to apply advanced longitudinal methods to facilitate understanding of individual progression of rehabilitation outcomes. This symposium will describe the conceptual model for evaluating outcomes as trajectories of recovery, and present results from three longitudinal stroke rehabilitation studies to demonstrate clinical applications and interpretations of longitudinal mixed effects regression models. Results of each study will be discussed in the context of clinical applications and implications.
Increasing Communication Access for Patients in Rehabilitation Settings: Interdisciplinary Perspectives on Communication Partner Training (843181)
Presenters: Elissa Larkin Conlon, MS, CCC-SLP, Kristen Gracz, MSN, RN, CNL, CRRN, Viktoriya Landar, OTR/L, Leora R. Cherney, PhD, CCC-SLP, BC-ANCDS, FACRM moderator
In order to maximize outcomes, rehabilitation clinicians must be able to communicate effectively with patients. However, many patients face barriers that impact their communication; related to their diagnosis, health literacy, or primary language. Although there are evidence-based methods to support effective patient communication, few providers receive explicit training on these techniques. This session will first provide a condensed communication partner training highlighting evidence-based communication strategies most relevant to rehabilitation practice. Presenters will then provide an overview of two training models implemented successfully in a rehabilitation hospital system with and Nursing staff. Trainees from each program will describe their respective experiences and share pilot effectiveness data. Finally, audience participants will engage in a collaborative discussion of considerations for tailoring communication partner training programs to the unique needs of their own diverse rehabilitation teams and their patients.