IISIG Webinar
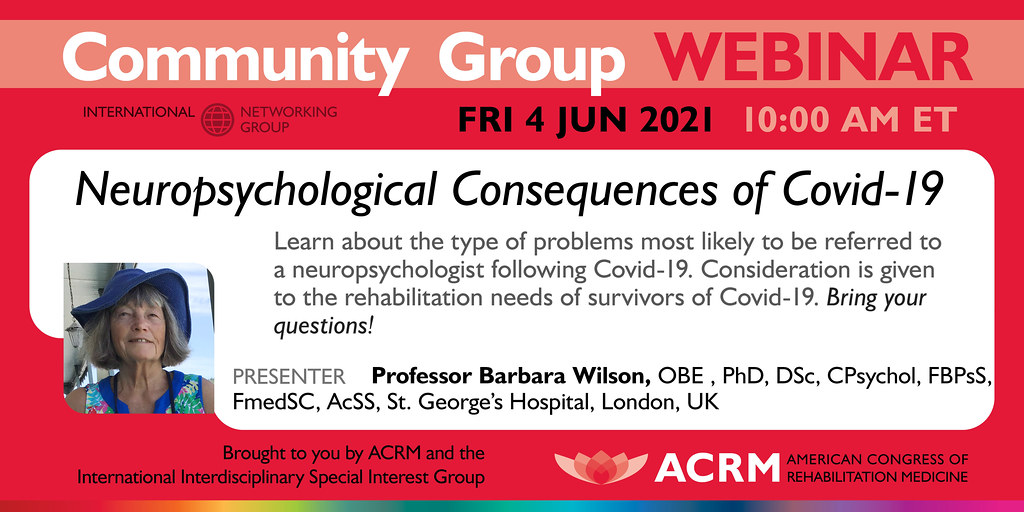
Neuropsychological Consequences of Covid-19
WITH GUEST SPEAKER, PROFESSOR BARBARA WILSON, OBE, PHD,DSC, CPSYCHOL, FBPSS, FMEDSC, ACSS
4 JUNE // 10:00 – 11:00 AM ET
Although we know a considerable amount about the medical aspects of the new corona virus, SARS-Covid-2 and the illness it causes namely Covid-19, less is known about the neuropsychological aspects. There indications that strokes, encephalitis and hypoxia may occur after Covid-19 and that, in addition to the well-acknowledged difficulties with fatigue and deconditioning, people who have been severely ill may have cognitive, emotional and behavioural problems that require a referral to neuropsychology and/or neuropsychiatry services. We report on 70 patients referred to neuropsychology at St George’s Hospital, London. The age range was 32 to 84 years with a mean of 57 years. Men outnumbered women by over 2 to 1 and there were far more ethnic minority patients than seen in the general population served by St George’s hospital. The majority of patients were referred for assessment of cognitive and mood problems with a smaller number referred for other reasons such as whether referral to another unit was acceptable, attention seeking behaviour and for non-specific reasons. The cognitive problems noted most frequently were with memory, executive functions and slow information processing. Emotional or psychological problems included anxiety, sleep problems and anger. Just over 8 per cent developed a stroke as a result of Covid-19. Many had underlying health problems including a previous stroke, diabetes, HIV and sickle-cell disease. In addition to the neuropsychological problems identified, about 10 per cent of survivors required dialysis for kidney failure and a similar number were left with cardiac difficulties. We have just started to follow-up these people in order to determine whether their difficulties persist or resolve over time.
Learning Objectives
Upon completion of the webinar, learners will be able to:
- Describe problems most likely to be referred to a neuropsychologist following Covid-19.
- Understand that ethnic minorities are more at risk of becoming seriously ill than their white British counterparts.
- Discuss the unique rehabilitation needs of survivors of Covid-19.
ABOUT BARBARA WILSON
Barbara Wilson is a clinical neuropsychologist who has worked in brain injury rehabilitation for 43 years. She has published 32 books, 204 peer reviewed papers, 124 chapters and 8 neuropsychological tests. She has won many awards for her work including an OBE from the Queen in 1998, for services to rehabilitation; five lifetime achievement awards, one from the British Psychological Society, one from the International Neuropsychological Society, one from the National Academy of Neuropsychology, one from the Encephalitis Society and one from the NHS 70 year anniversary parliamentary awards where she was regional champion for the Midlands and East Region. In 2011 she received the Ramon Y Cahal award from the International Neuropsychiatric Association. In 2014 she received an honorary degree from The University of Cordoba, Argentina. Also in 2014 she received the M.B. Shapiro award from The Division of Clinical Psychology (affiliated to The British Psychological Society) for Distinguished Contributions to Clinical Psychology. In 2019 she received the annual award from the Spanish Clinical Neuropsychological Society. She is editor of the journal “Neuropsychological Rehabilitation” which she founded in 1991 and in 1996 she established the Oliver Zangwill Centre for Neuropsychological Rehabilitation. A rehabilitation centre in Quito, Ecuador is named after her. She is president emeritus of the UK Encephalitis Society and is on the management committee of The World Federation of Neuro Rehabilitation. The UK Division of Neuropsychology has named a prize after her, the ‘Barbara A Wilson prize for distinguished contributions to neuropsychology’. She is a Fellow of The British Psychological Society, The Academy of Medical Sciences and The Academy of Social Sciences. She is honorary professor at the University of Hong Kong, the University of Sydney and the University of East Anglia. She has held 30 research grants. Her work has resulted in changes in clinical practice. For example, as a result of a randomised control trial evaluating a paging system to improve the everyday functioning of people with memory and planning problems, the local health authority set this up as a health care system for people throughout the United Kingdom. She is currently working free lance for St George’s Hospital in London on the neuropsychological consequences of Covid-19 and, occasionally, for the Oliver Zangwill Centre.











