2019 Conference Highlights
View Special Symposia >>
View Hot Topics in Stroke >>
View Instructional Courses >>
Join Us In Chicago!
All conference attendees are automatically ACRM members. Non-members receive a 6-month introductory ACRM membership automatically with registration. Put your member benefits to work right away—join an ACRM community group and attend a community group or task force meeting! PLEASE NOTE: Dates and times are subject to change. Please check the Online Program for the most up-to-date information.
Tuesday 5 NOV
9:30 AM – 10:30 AM
- Stroke-ISIG Aphasia and Other Communication Disorders Task Force Meeting (open for ALL to attend)
Location: 4L, 4th Floor
Wednesday 6 NOV
7:00 AM – 8:00 AM
- Stroke-ISIG Pediatric Stroke Task Force Meeting (open for ALL to attend)
Location: 4L, 4th Floor
8:00 PM – 9:00 PM
- Stroke-ISIG Movement Task Force Meeting (open for ALL to attend)
Location: 4E, 4th Floor
Thursday 7 NOV
7:00 AM – 8:00 AM
- Stroke-ISIG Annual Business Meeting (open for ALL to attend)
Location: 4D, 4th Floor
Friday 8 NOV
7:00 AM – 8:00 AM
- Stroke-ISIG Transitions & Continuity of Care Task Force Meeting (open for ALL to attend)
Location: 4I, 4th Floor
Special Symposia >>
SPECIAL SYMPOSIUM & ASA/ACRM Award for Excellence in Post-Acute Stroke Rehabilitation: Biomarkers in Stroke Recovery and Rehabilitation Research >>

A number of therapies are emerging that aim to promote favorable brain plasticity after stroke, with the goal being to improve outcomes and reduce disability. Treating the brain is not a “one-size-fits-all” process. Instead, certain treatments are more, or less, likely to improve brain function in specific subsets of patients. This presentation will briefly review the range of therapies under study, then focus on measurements that have been evaluated for predicting responders versus non-responders in the context of restorative therapies after stroke, with an emphasis on studies targeting the motor system.
Learn more >>
Hot Topics in Stroke
HOT TOPICS IN STROKE: Inconsistent Classification of Mild Stroke and Implications of Health Service Delivery >>
Patients classified with mild stroke typically do not receive treatment or rehabilitation services but may experience deficits months following stroke. Lack of a global consensus on the definition of mild stroke may result in variability in treatment during acute care and outcomes following discharge. For this hot topic panel discussion, an interdisciplinary team of clinicians and researchers will discuss the clinical and outcome assessments used internationally to classify stroke severity, the need for an international consensus definition, and the implications of inconsistent classification on health service delivery following a mild stroke.
Learn more >>
HOT TOPICS IN STROKE: Young Stroke and Complex Needs Across the Care Continuum >>
Stroke in young adults is a major issue in the United States. Although the appreciation for the complexities associated with young stroke rehabilitation have been recognized, this population experiences complex and dynamic needs that may not be supported by current systems of care. In fact, stroke rehabilitation in the United States is often fragmented which contributes to challenges with comprehensive and coordinated care. This is particularly problematic during transitions of care and after discharge to the community. The invited speakers will discuss young stroke, transitions of care, discharge preparedness, and an ongoing needs assessment being conducted.
Learn more >>
Instructional Courses >>
IC 5: Interdisciplinary Perspectives to Functional Measurement and Assessment of the Stroke Survivor >>
Stroke is one of the leading causes of disability in the United States. Given stroke can affect all aspects of bodily function and abilities, multiple measurements and assessments are administered across disciplines. These measurements are critical in evaluating function and providing effective care for the stroke survivor. Clinical knowledge of various standardized assessments is required of all medical professionals to create effective goals for stroke patients to achieve functional outcomes.
Learn more >>
IC 6: Wheelchairs and Seating: The Evaluation Process with Demonstration and Justification of Recommended Products >>
The purchase of a wheelchair and seating products is a critical step for many non-ambulatory individuals. This hands-on course provides evaluation techniques, product demonstration, and funding criteria for individuals of all ages having a variety of neurological or orthopedic diagnoses. It will provide a step-by-step overview beginning with the medical intake and information gathering pertaining to physical and functional parameters for decision making. The mat evaluation and measurements, will be covered. Participants will learn how to perform an evaluation, fill out a detailed form with medical justification of the products, and trial mobility bases, cushions, and supports.
Learn more >>
IC 1A: The Experience of Individuals with ABI and their Families: Family Intervention in the Rehabilitation Setting >>
Acquired brain injuries (ABI) can have deleterious effects on family life,often changing roles and routines, and fostering intense and prolonged caregiving duties. Individuals with ABI and their partners may experience Increased familial distress, marital strain, reduced sexual intimacy and overall disatisfaction with the relationship. Yet, healthcare professionals are unsure on how to most effectively intervene to improve problem solving, communication, affective responsiveness, affective involvement, and behavioral control within the family unit. This workshop aims to introduce a manualized culturally competent intervention appraoch of family systems developed by Juan Carlos Arango-Lasprilla, PhD. & colleagues, for use in the rehabilitation setting.
Learn more >>
IC 16: Improving Balance Control and Preventing Falls: Evidence-Based Approaches for Adult Neurological Populations >>

Falls and impaired balance are a significant concern for individuals living with neurological conditions, and neurological rehabilitation programs are evolving in order to target these issues. In this evidence-based instructional course you will learn how to: 1) implement a framework for an individualized assessment of fall risk; 2) develop individualized fall prevention strategies for people living with a neurological condition; 3) assess the various systems of balance control through bedside and instrumented approaches; and, 4) deliver comprehensive balance training and appreciate the ability of technology, such as functional electrical stimulation, to augment these training approaches.
Learn more >>
IC 19: Building Your Toolkit to Address Sexuality and Intimacy After Brain Injury >>
This workshop on sexuality and intimacy in brain injury rehabilitation has been developed to reduce stigma and build knowledge, imparting an increase in comfort that leads to action in addressing the topic for our patients. Content shared will include: biopsychosocial factors, sexual dysfunction and the impact on the person with a brain injury and their partners, cultural and interpersonal aspects to consider, and communication strategies to employ. Throughout the workshop, attendees will participate in reflection on current practice and potential biases, as well as institutional practices and policies. Upon completion of the workshop, attendees will come away with tools to facilitate change in practice within their organization.
Learn more >>
IC 20: Functional Assessment and Prism Adaptation Treatment for Spatial Neglect after Stroke >>
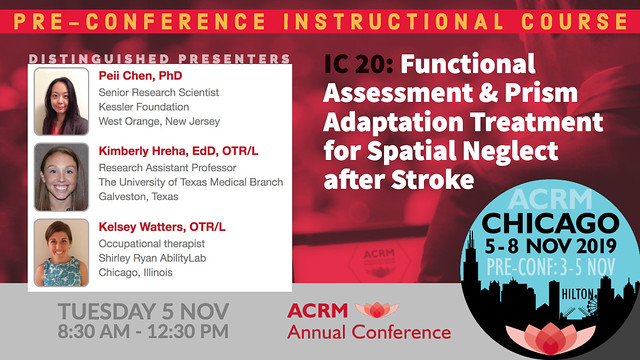
In this instructional course, we will first discuss the definition of spatial neglect and emphasize the clinical impact on stroke survivors. Next, we will explain the KF-NAP and offer participants the opportunity to practice using the assessment through access to patient cases via video. After, the KF-PAT will be introduced. Small groups will now learn to administer this treatment protocol by actually practicing with the equipment. Conclusions will be a discussion the practical implications of using both protocols in an inpatient rehabilitation facility.
Learn more >>
LEARN MORE | REGISTER | BOOK HOTEL | ONLINE PROGRAM
ACRM 96th Annual Conference | Progress in Rehabilitation Research
CORE: 5 – 8 NOV 2019 // CHICAGO USA // PRE-CONFERENCE: 3 – 5 NOV 2019









